Refractory Shock
Dr. Amanda Berggren
University of Colorado, PGY-6
Case:
A 72-year-old female presents to the emergency department (ED) with a chief complaint of fatigue. Her symptoms have been progressing over the last two days. She has been unable to get out of bed, and her family found her minimally responsive this morning. She was reported to be in her usual state of health up until two days ago when she started feeling unwell. She does not remember if she has been taking her medications. She has had minimal oral intake and decreased urine output. The remainder of the history is limited, and there is no collateral information immediately available. Her workup reveals multiple infiltrates on chest x-ray, elevated white blood cell count, and elevated lactate. Her vitals are notable for tachycardia, hypotension, and fever.
This patient’s initial workup is concerning for septic shock. The patient is started on broad spectrum antibiotics and receives 2L of crystalloid without improvement. Peripheral norepinephrine is started and rapidly uptitrated to 1 mcg/kg/min, but the patient remains hypotensive. Vasopressin is added at 0.03 unit/min, and the emergency physician decides to place a central line and arterial line while awaiting ICU placement. What are the next steps for this patient with refractory shock?
Refractory shock is a state of shock that persists despite the administration of high doses of vasopressor medication, defined by the 2021 Surviving Sepsis Campaign as norepinephrine or epinephrine ³ 0.25 µg/kg/min for at least 4 hours.1 Patients will have persistent hypotension and end-organ hypoperfusion due to inadequate hemodynamic response to these medications. This condition carries a high mortality, necessitating aggressive interventions.
Vasoactive medications are the mainstay of treatment of refractory shock, but there is heterogenous evidence regarding the various vasopressors and inotropes used in the management of shock. In this section, we will discuss the advanced applications of the most used vasoactive agents in the management of refractory shock.
Norepinephrine is typically the first-line vasopressor for most patients. Norepinephrine targets both a and b-adrenergic receptors, with a more pronounced impact on a receptors. These effects result in vasoconstriction, an increased heart rate, and improved contractility. The maximum dose of norepinephrine is not universally standard, or is norepinephrine standardly dosed between institutions. Numerous studies have associated high-dose norepinephrine with increased mortality rates, although almost every study differs as to the definition of high-dose. While the surviving sepsis campaign identifies high-dose norepinephrine as 0.25 µg/kg/min for at least 4 hours, there are alternative studies that define high-dose norepinephrine as 0.4 µg/kg/min or even 1 µg/kg/min. A retrospective review identified an increased mortality when infusion rates of norepinephrine reached and surpassed 18 µcg/min.2 In another study, doses exceeding 1µg/kg/min were associated with a 90% mortality. 3 It is important to note that these patients have conditions, like septic shock, that are already increasing their mortality risk. If increasing past these hypothetical ceiling doses, it is important to consider the risks of mesenteric and digital ischemia. There should be careful consideration of the risks and benefits of continuing to uptitrate vasopressors in patients with refractory shock.
While bolus-dose epinephrine is the primary choice in cardiac arrest, it is not used as frequently in shock. Epinephrine also targets both a and b receptors, resulting in increased systemic vascular resistance (SVR) and positive inotropic and chronotropic effects. At lower doses, epinephrine primarily acts as an inotrope by activating b-1 receptors. At higher doses, epinephrine affects a-1 receptors leading to an increase in cardiac output and SVR. The dose definitions are not perfectly defined, but the literature supports “low dose” as 0.01-0.05 µg/kg/min and “high dose” as 0.1 µg/kg/min or higher.4 The use of epinephrine in shock has been influenced by several studies comparing it to norepinephrine in both septic and cardiogenic shock. Although these studies show epinephrine is as effective as norepinephrine in achieving MAP goals, there may be increased drug-related side effects with epinephrine.5-7 These adverse effects include arrhythmias and lactic acidosis. These effects underscore the preference for norepinephrine as the first-line vasopressor in shock management, as recommended by the Society of Critical Care Medicine in the Surviving Sepsis Campaign guidelines.1
There are limited indications for phenylephrine as a first-line agent. Phenylephrine acts selectively on the a-1 adrenergic receptors, thereby increasing SVR and MAP without significant tachycardia and, sometimes, with reflex bradycardia. This makes it an attractive agent for clinical scenarios in which tachycardia causes significant worsening hemodynamics. For example, in patients with hypertrophic cardiomyopathy with acute hypotension, phenylephrine is the recommended vasopressor as it helps optimize preload and afterload without increasing contractility or heart rate, thus avoiding left ventricular outflow tract obstruction.7 Another use of phenylephrine is seen in the management of cardiogenic shock in the context of mitral stenosis. The increase in SVR without the increase in heart rate allows for improved diastolic filling time and cardiac output.8 While reflex bradycardia may be a welcomed side effect in mitral stenosis, be mindful of its potential negative impact on overall hemodynamic stability in other patient populations.
Vasopressin is frequently chosen as a second-line vasopressor after norepinephrine in septic shock but has utility in other etiologies of shock as well. Vasopressin acts as a potent vasoconstrictor through its action on the V1 receptors on vascular smooth muscle cells. The VASST and VANISH trials are two important studies regarding vasopressin use in septic shock. Although neither study found significant improvement in 28-day mortality, there was improved survival in patients receiving lower dose norepinephrine (< 15 µg/min) when vasopressin was added and a reduced risk of renal replacement therapy (RRT), respectively.9,10 Conversely, the VANCS trial showed a significant reduction in mortality or 30-day severe complications with the use of vasopressin compared to norepinephrine in vasoplegic shock post-cardiac surgery.11 It is important to note the different dosing strategies between these two etiologies of shock. For septic shock, the Surviving Sepsis Campaign guidelines recommend starting vasopressin as a dose of 0.03 units/min as an adjunct to norepinephrine when dosage reaches 0.25-0.5 µg/kg/min,12 reflecting that the survival benefit of adding vasopressin to norepinephrine in the VASST trial was for patients requiring less than 15 µg/min of norepinephrine.9 For vasoplegic shock after cardiac surgery, the recommended dosing range is 0.03 to 0.1 units/min.11 Like previous vasopressors discussed, vasopressin carries the risk of complications. Cardiac, digital, and mesenteric ischemia are all risks that should be monitored for while utilizing vasopressin.7 The splanchnic vasoconstrictive effects of vasopressin become beneficial in managing patients with acute gastrointestinal hemorrhage from variceal bleeding.12
With regards to inotropes, there are two that are most commonly used: dobutamine and milrinone. Dobutamine primarily stimulates b-1 adrenergic receptors, enhancing cardiac contractility, and to a lesser extent a-1 adrenergic receptors, influencing vascular tone. Low dose dobutamine (less than 5 µg/kg/min) may cause a decrease in SVR, whereas high dose dobutamine (greater than 10 µg/kg/min) can increase SVR as well as increase the risk of tachycardia.13,14 Milrinone acts as a phosphodiesterase III inhibitor, effectively mimicking b-1 and b-2 receptor activation without directly stimulating these receptors. Both agents are commonly used in cardiogenic shock. A 2021 study in the New England Journal of Medicine compared the two and found no significant difference in terms of in-hospital mortality, receipt of a cardiac transplant, nonfatal myocardial infarction, stroke, or initiation of RRT.15 It is important to note that milrinone is primarily excreted by the kidneys, and renal impairment prolongs its elimination half-life and increases the risk for side effects. One cohort of patients to consider milrinone over dobutamine is those on a nonselective beta-blocker. Milrinone maintains efficacy despite beta-blocker therapy, where dobutamine required higher doses that were associated with adverse effects.16 Although inotropic agents are not frequently utilized in the management of septic shock, it could be considered in a patient with septic shock who is refractory to conventional resuscitation and vasopressor therapies. One study indicates sepsis-induced cardiomyopathy, defined as an ejection fraction < 50% and a ≥ 10% decrease compared to baseline ejection fraction, occurs in 13.8% of patients with sepsis and septic shock.17 In the context of septic shock, no significant in hospital mortality was identified between dobutamine versus milrinone, but milrinone may be associated with higher rates of RRT and longer hospital stays.18
Angiotensin II is a newer vasoactive agent that may be used in cases of refractory shock. Angiotensin II binds to the AT II receptors on vascular smooth muscles causing vasoconstriction and stimulates the release of aldosterone. The ATHOS-3 trial in 2017 was a randomized controlled trial that showed angiotensin II significantly increased MAP in patients with refractory vasodilatory shock when compared to the placebo group.19 After this pivotal trial, several additional reviews looked at the use of angiotensin II for refractory shock. Several of these studies showed a favorable hemodynamic response to angiotensin II with increased MAP and a reduction in vasopressor requirements, but there was no significant improvement in mortality.20,21 These studies also indicate the most benefit with angiotensin II is seen in patients with acute kidney injury requiring RRT and those with lower lactate levels or on vasopressin.20,22 Ischemic side effects are still seen with angiotensin II like with other vasopressors. The patients receiving angiotensin II in the ATHOS-3 trial also experienced a higher number of thromboembolic events compared to the control group (12.9% versus 5.1%).19 This highlights the need for careful patient consideration before starting angiotensin II, and the recommendation to administer venous thromboembolism prophylaxis to these patients.
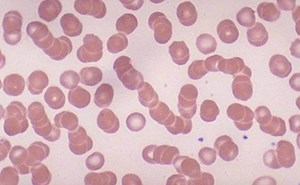
Beyond traditional vasopressors and inotropes, there are other pharmacologic agents to assist with refractory shock. Methylene blue is another agent to consider in the management of refractory shock. Methylene blue is used in the treatment of methemoglobinemia, but it also improves vasoconstriction by inhibiting nitric oxide synthase and guanylate cyclase, thereby reducing nitric oxide production.23 Clinical evidence supports the efficacy of methylene blue in improving hemodynamics and reducing vasopressor requirements, thereby significantly reducing mortality in patients with vasodilatory shock.24,25 This evidence is fairly recent, and more information is required to make methylene blue a regular agent in the treatment of shock, but it should be considered in cases of catecholamine-resistant shock. There are some adverse effects to consider before ordering methylene blue. Methylene blue will turn the urine blue and lead to possible blue skin discoloration, as well as possibly induce a rapid and significant drop in pulse oximetry readings.26 While these effects are temporary and benign, it can be disconcerting. There are more serious concerns when using methylene blue, including the risk of serotonin syndrome in patients with concomitant use of serotonergic drugs.27 The other significant concern is in patients with glucose-6-phosphate dehydrogenase (G6PD) deficiency, as hemolytic anemia can be seen.28 These side effects highlight the importance of reviewing medical history and medications prior to using methylene blue.
Hydroxycobalamin is another nitric oxide synthase inhibitor that has been used in the setting of distributive shock. The added benefit of hydroxycobalamin is the inhibition of hydrogen sulfide, which also contributes to vasodilation. Evidence suggests that hydroxycobalamin improves hemodynamics and reduces vasopressor requirements, but there is no conclusive evidence that it decreases mortality.29 Hydroxycobalamin administration comes with adverse effects that providers need to be aware of before use. While it causes transient, red-colored urine and erythema which may be surprising to see while assessing a patient, the color change impacts dialysis machines as well as colorimetric laboratory assays.30
There are no direct comparison studies between methylene blue and hydroxycobalamin in septic shock, but retrospective data analysis and a post-cardiac surgery vasoplegic shock study provide some evidence comparing the two. Both agents have efficacy in managing refractory shock, but some evidence suggests hydroxycobalamin may have superior hemodynamic benefits, while methylene blue has been associated with reduced mortality in critically ill patients.31 When choosing between these two agents, it is important to consider adverse effects and concurrent medications and co-morbidities.
Steroids play a significant role in the management of refractory shock and improve survival in specific patient populations. The typical regimen recommended is 200 mg/day of intravenous hydrocortisone, given as 50 mg every 6 hours.1 Clinical trials and studies have shown that hydrocortisone can improve mortality in patients with septic shock requiring high-dose vasopressors.32 Additional studies suggest that hydrocortisone may be particularly beneficial in patients with relative adrenal insufficiency, which is common in patients with cirrhosis and septic shock.33 The combination of hydrocortisone and fludrocortisone was studied in the APROCCHSS trial. This trial demonstrated that the addition of fludrocortisone significantly reduced 90-day all-cause mortality and increased the number of vasopressor-free days.34 The recommended dose of fludrocortisone is 50 mg daily.
Mechanical circulatory support (MCS) is used in cases of refractory shock when initial therapies are insufficient to achieve hemodynamic stability. The utility is primarily in cases of cardiogenic shock or rare cases of septic shock with a component of sepsis-induced cardiomyopathy. The American College of Cardiology guidelines support the use of temporary MCS in patients with cardiogenic shock who are at risk of multi-organ failure who cannot be managed with intravenous inotropes or vasopressors alone.35 The Surviving Sepsis Campaign does not provide a strong recommendation for MCS in septic shock due to limited evidence,1 and outcomes for adult patients with isolated distributive shock are very poor. MCS devices include intra-aortic balloon pumps (IABP), microaxial flow pumps, ventricular assist devices (VAD), and extracorporeal membrane oxygenation (ECMO). The rationale behind MCS is to provide immediate hemodynamic support offering a bridge to recovery or definitive therapy. A network meta-analysis suggests that ECMO-IABP therapy has the most promise in reducing mortality.36
A multidisciplinary team approach is crucial for managing refractory shock and it is important to know your hospital’s protocols and capabilities. There is ongoing research regarding various vasopressors and their optimal use in managing refractory shock. Active studies are investigating patient outcomes when utilizing vasopressin, angiotensin II, and inotropes. As new evidence emerges, changes to recommendations and practices may arise.
References:
- Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021;47(11):1181-1247. doi:10.1007/s00134-021-06506-y
- Singer KE, Sussman JE, Kodali RA, et al. Hitting the vasopressor ceiling: Finding norepinephrine associated mortality in the critically ill. J Surg Res. 2021;265:139-146. doi:10.1016/j.jss.2021.03.042
- Martin C, Medam S, Antonini F, et al. Norepinephrine: Not Too Much, Too Long. Shock. 2015;44(4):305-309. doi:10.1097/SHK.0000000000000426
- Zimmerman J, Cahalan M. Vasopressors and inotropes. In: Hemmings HC, Egan TD, eds. Pharmacology and Physiology for Anesthesia. Philadelphia, PA: W.B. Saunders; 2013:390-404. doi:10.1016/B978-1-4377-1679-5.00022-3
- Myburgh JA, Higgins A, Jovanovska A, et al. A comparison of epinephrine and norepinephrine in critically ill patients. Intensive Care Med. 2008;34(12):2226-2234. doi:10.1007/s00134-008-1219-0
- Levy B, Perez P, Perny J, et al. Comparison of norepinephrine-dobutamine to epinephrine for hemodynamics, lactate metabolism, and organ function variables in cardiogenic shock. A prospective, randomized pilot study. Crit Care Med. 2011;39(3):450-455. doi:10.1097/CCM.0b013e3181ffe0eb
- Levy B, Clere-Jehl R, Legras A, et al. Epinephrine Versus Norepinephrine for Cardiogenic Shock After Acute Myocardial Infarction. J Am Coll Cardiol. 2018;72(2):173-182. doi:10.1016/j.jacc.2018.04.051
- Ommen SR, Ho CY, Asif IM, et al. 2024 AHA/ACC/AMSSM/HRS/PACES/SCMR Guideline for the Management of Hypertrophic Cardiomyopathy: A Report of the American Heart Association/American College of Cardiology Joint Committee on Clinical Practice Guidelines [published correction appears in Circulation. 2024 Aug 20;150(8):e198. doi: 10.1161/CIR.0000000000001277.]. Circulation. 2024;149(23):e1239-e1311. doi:10.1161/CIR.0000000000001250
- Gutierrez EJ. The Vasopressor & Inotrope Handbook: A Practical Guide for Healthcare Professionals. Independently published; 2023.
- Russell JA, Walley KR, Singer J, et al. Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med. 2008;358(9):877-887. doi:10.1056/NEJMoa067373
- Gordon AC, Mason AJ, Thirunavukkarasu N, et al. Effect of Early Vasopressin vs Norepinephrine on Kidney Failure in Patients With Septic Shock: The VANISH Randomized Clinical Trial. JAMA. 2016;316(5):509-518. doi:10.1001/jama.2016.10485
- Hajjar LA, Vincent JL, Barbosa Gomes Galas FR, et al. Vasopressin versus Norepinephrine in Patients with Vasoplegic Shock after Cardiac Surgery: The VANCS Randomized Controlled Trial. Anesthesiology. 2017;126(1):85-93. doi:10.1097/ALN.0000000000001434
- Garcia-Tsao G, Sanyal AJ, Grace ND, et al. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Am J Gastroenterol. 2007;102(9):2086-2102.
- Pinaud M, Desjars P, Nicolas F. Dobutamine in the treatment of depressed cardiac function: a study in patients with ischaemic heart disease during the early post-operative period. Intensive Care Med. 1978;4(2):105-110. doi:10.1007/BF01684395
- Andy JJ, Curry CL, Ali N, et al. Cardiovascular effects of dobutamine in severe congestive heart failure. Am Heart J. 1977;94(2):175-182. doi:10.1016/s0002-8703(77)80277-9
- Mathew R, Di Santo P, Jung RG, et al. Milrinone as Compared with Dobutamine in the Treatment of Cardiogenic Shock. N Engl J Med. 2021;385(6):516-525. doi:10.1056/NEJMoa2026845
- Lowes BD, Tsvetkova T, Eichhorn EJ, et al. Milrinone versus dobutamine in heart failure subjects treated chronically with carvedilol. Int J Cardiol. 2001;81(2-3):141-149. doi:10.1016/s0167-5273(01)00520-4
- Sato R, Kuriyama A, Takada T, et al. Prevalence and risk factors of sepsis-induced cardiomyopathy: A retrospective cohort study. Medicine (Baltimore). 2016;95(39):e5031. doi:10.1097/MD.0000000000005031
- Zhu Y, Yin H, Zhang R, et al. The effect of dobutamine vs milrinone in sepsis: A big data, real-world study. Int J Clin Pract. 2021;75(11):e14689. doi:10.1111/ijcp.14689
- Khanna A, English SW, Wang XS, et al. Angiotensin II for the Treatment of Vasodilatory Shock. N Engl J Med. 2017;377(5):419-430. doi:10.1056/NEJMoa1704154
- Wieruszewski PM, Wittwer ED, Kashani KB, et al. Angiotensin II Infusion for Shock: A Multicenter Study of Postmarketing Use. Chest. 2021;159(2):596-605. doi:10.1016/j.chest.2020.08.2074
- Xourgia E, Exadaktylos AK, Chalkias A, et al. Angiotensin II in the treatment of distributive shock: a systematic-review and meta-analysis. Shock. 2024;62(2):155-164. doi:10.1097/SHK.0000000000002384
- Tumlin JA, Murugan R, Deane AM, et al. Outcomes in Patients with Vasodilatory Shock and Renal Replacement Therapy Treated with Intravenous Angiotensin II [published correction appears in Crit Care Med. 2018 Aug;46(8):e824. doi: 10.1097/CCM.0000000000003226.]. Crit Care Med. 2018;46(6):949-957. doi:10.1097/CCM.0000000000003092
- Ballarin RS, Lazzarin T, Zornoff L, et al. Methylene blue in sepsis and septic shock: a systematic review and meta-analysis. Front Med (Lausanne). 2024;11:1366062. Published 2024 Apr 18. doi:10.3389/fmed.2024.1366062
- Pruna A, Bonaccorso A, Belletti A, et al. Methylene Blue Reduces Mortality in Critically Ill and Perioperative Patients: A Meta-Analysis of Randomized Trials. J Cardiothorac Vasc Anesth. 2024;38(1):268-274. doi:10.1053/j.jvca.2023.09.037
- Zhao CC, Zhai YJ, Hu ZJ, et al. Efficacy and safety of methylene blue in patients with vasodilatory shock: A systematic review and meta-analysis. Front Med (Lausanne). 2022;9:950596. Published 2022 Sep 26. doi:10.3389/fmed.2022.950596
- Rong LQ, Mauer E, Mustapich TL, et al. Characterization of the Rapid Drop in Pulse Oximetry Reading After Intraoperative Administration of Methylene Blue in Open Thoracoabdominal Aortic Repairs. Anesth Analg. 2019;129(5):e142-e145. doi:10.1213/ANE.0000000000004325
- Basta MN. Postoperative serotonin syndrome following methylene blue administration for vasoplegia after cardiac surgery: a case report and review of the literature. Semin Cardiothorac Vasc Anesth. 2021;25(1):51-56. doi:10.1177/1089253220960255
- Youngster I, Arcavi L, Schechmaster R, et al. Medications and glucose-6-phosphate dehydrogenase deficiency: an evidence-based review. Drug Saf. 2010;33(9):713-726. doi:10.2165/11536520-000000000-00000
- Patel JJ, Willoughby R, Peterson J, et al. High-Dose IV Hydroxocobalamin (Vitamin B12) in Septic Shock: A Double-Blind, Allocation-Concealed, Placebo-Controlled Single-Center Pilot Randomized Controlled Trial (The Intravenous Hydroxocobalamin in Septic Shock Trial). Chest. 2023;163(2):303-312. doi:10.1016/j.chest.2022.09.021
- Food and Drug Administration. Updated April 27, 2023. Accessed [Dec 16, 2024]. https://www.accessdata.fda.gov/drugsatfda_docs/label/2018/022041s019,%20020lbl.pdf
- Hiruy A, Ciapala S, Donaldson C, et al. Hydroxocobalamin Versus Methylene Blue for the Treatment of Vasoplegic Shock Associated With Cardiopulmonary Bypass. J Cardiothorac Vasc Anesth. 2023;37(11):2228-2235. doi:10.1053/j.jvca.2023.07.015
- Karvellas CJ, Bajaj JS, Kamath PS, et al. AASLD Practice Guidance on Acute-on-chronic liver failure and the management of critically ill patients with cirrhosis. Hepatology. 2024;79(6):1463-1502. doi:10.1097/HEP.0000000000000671
- Fernández J, Escorsell A, Zabalza M, et al. Adrenal insufficiency in patients with cirrhosis and septic shock: Effect of treatment with hydrocortisone on survival. Hepatology. 2006;44(5):1288-1295. doi:10.1002/hep.21352
- Annane D, Renault A, Brun-Buisson C, et al. Hydrocortisone plus Fludrocortisone for Adults with Septic Shock. N Engl J Med. 2018;378(9):809-818. doi:10.1056/NEJMoa1705716
- Heidenreich PA, Bozkurt B, Aguilar D, et al. 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure: A Report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines [published correction appears in J Am Coll Cardiol. 2023 Apr 18;81(15):1551. doi: 10.1016/j.jacc.2023.03.002.]. J Am Coll Cardiol. 2022;79(17):e263-e421. doi:10.1016/j.jacc.2021.12.012
- Low CJW, Ling RR, Lau MPXL, et al. Mechanical circulatory support for cardiogenic shock: a network meta-analysis of randomized controlled trials and propensity score-matched studies. Intensive Care Med. 2024;50(2):209-221. doi:10.1007/s00134-023-07278-3