Acute Liver Failure – A Snapshot Review
Dr. Remy Arnot, PGY-2
University of Arizona, Emergency Medicine Residency
Acute liver failure (ALF) is a rare disorder with a high mortality.1 ALF is defined by a severe, acute (categorized as less than 26 weeks in duration) liver injury associated with coagulopathy (INR ≥1.5), transaminitis, and hepatic encephalopathy in a person without known underlying liver disease.2 For those that do not spontaneously recover with supportive care, liver transplant is the only definitive treatment, without which life expectancy may be less than seven days.3 Whenever possible, patients with ALF should be managed at a center capable of hepatic transplant.
Demographics/Etiology
The most common cause of ALF in developed countries is drug induced liver injury, while the most common cause of ALF in developing countries is viral hepatitis.1 In the United States, acetaminophen overdose remains the most common cause of ALF, although other drugs can also be a culprit. With regards to viral etiologies, the hepatitis viruses A-E are common causes, with hepatitis B the most common of the five. However, ALF can also be seen with other viruses such as adenovirus, Epstein-Barr virus, herpes simplex virus, and varicella zoster virus.
Presentation
Patients with ALF may present to the emergency department with a variety of symptoms. This includes fatigue, lethargy, nausea, vomiting, abdominal pain, jaundice, or pruritis. With regards to the neurologic manifestations of ALF, patients may present within a spectrum of encephalopathy. The severity of hepatic encephalopathy can be defined by the West-Haven Criteria, ranging from poor attention span (Grade I) to coma (Grade IV).2 In ALF, the ammonia level is directly related to the severity of hepatic encephalopathy, with sustained levels >150 umol/L associated with worse outcomes.4 The osmotic gradient established by ammonia in glial cells drives cerebral edema and causes a subsequent increase in intracranial cranial pressure (ICP), which is directly associated with mortality.5 Cerebral edema is often present in patients with grade III or IV encephalopathy which is associated with somnolence, confusion, gross disorientation, and bizarre behavior.2
Diagnosis & Treatment
Patients without a history of liver disease who come in with altered mental status and are found to have a severe transaminitis (25x the upper limit of normal) and coagulopathy (INR>1.5) should be suspected to have ALF. A pre-existing diagnosis of liver disease excludes a patient from having ALF. Initial laboratory workup should rule out chronic liver diseases and reversable causes of liver disease, such as auto-immune conditions, obstructive conditions, and temporary physiologic processes, such as pregnancy. Liver function tests, coagulation panels, urine toxicology, and ammonia levels should be acquired immediately, including a pregnancy test if applicable. Additional lab tests to order include acetaminophen level, viral testing (hepatitis, EBV, HSV and CMV), copper studies and lipase.2
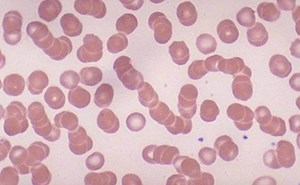
The INR may not accurately reflect bleeding risk in ALF patients, and viscoelastic testing should be considered. Most ALF patients experience a degree of coagulopathy with spontaneous hemorrhage occurring most commonly within the GI tract. H2 or PPI therapy is recommended as prophylaxis.
Correction of coagulopathy is not recommended unless there is active bleeding or a high-risk procedure.6 Liver biopsy may assist in ruling out infiltrative diseases and malignancy; however, this is not a routine part of the initial workup.2 Biopsy may also assist with prognosis.
With regards to imaging, a right upper quadrant ultrasound with dedicated vascular studies should be ordered. Early ultrasonographic findings of ALF may show homogenously decreased liver echogenicity, which will progressively become heterogeneous over time. Doppler assessment of hepatic vascularity is important to rule out reversible pathologies including Budd-Chiari, ischemic hepatitis, and portal vein thrombosis.6 On imaging, the liver may appear shrunken secondary to massive cortical damage and collapse, compared to chronic liver failure where the cortex is more irregular and nodular.2 Additional imaging that may be appropriate include CT imaging of the head, abdomen and pelvis.
Initial stabilization of the patient with ALF may require intubation and mechanical ventilation due to severe encephalopathy. Many patients with ALF will have low systemic vascular resistance and may also have fluid losses, resulting in a need for volume resuscitation or the use of vasopressors to maintain organ perfusion. Additional deterioration can occur quickly from cerebral edema, hypoglycemia, and shock.
West-Haven Criteria should be used to stratify degree of encephalopathy and initial disposition of patient, with ICU level of care recommended for those with grade 2 encephalopathy or above, and intubation considered for those patients at grades 3 or 4.2 For patients with clinically significant hyperammonemia, rifaximin and lactulose should be used in combination early in treatment. For severe cases of encephalopathy associated with cerebral edema, hypertonic saline is preferred over mannitol and should be used as a one-time dose only.6 In the ICU, for patients with severe hyperammonemia, continuous renal replacement therapy (CRRT) is often employed to rapidly decrease ammonia levels and hopefully prevent or ameliorate intracranial hypertension7. For patients who are hemodynamically unstable, CRRT is preferred over intermittent hemodialysis due to its lower risk of cardiovascular instability.6
For patients with signs and symptoms concerning for elevated ICP, the gold standard for intracranial pressure monitoring is an intraventricular catheter.8 However, in the setting of coagulopathy, noninvasive methods may be preferred due to elevated procedural risk. One such method is ocular ultrasound.5 As the sheath of the optic nerve is a direct extension of the subarachnoid space, its diameter can function as a surrogate marker of intracranial pressure.9 In this context, the optic sheath will demonstrate change before other traditional ocular findings of elevated ICP such as papilledema.9 Optic nerve sheath diameter >5.2 mm is associated with an ICP >20 mmHg, and adult diameters >5.0 mm are considered abnormal.8 Furthermore, change in optic nerve diameter is directly associated with outcome of treatment in ALF patients.5 The sensitivity and specificity for this method are >80% and >70%, respectively.5
In addition to supportive care, some targeted treatments exist for specific etiologies of ALF. Patients who suffer ALF from acetaminophen toxicity should receive N-acetylcysteine (NAC). Acetaminophen overdoses which present within four hours of ingestion, gastric decontamination with activated charcoal may be beneficial.6 After this four-hour window, and after systemic absorption of acetaminophen begins, medical treatment options are limited to NAC.2 The duration of NAC therapy is titrated to mental status and lab values and should be evaluated on a case-by-case basis. The use of NAC in non-acetaminophen related ALF is an area of active research and may be given empirically for patients with mixed or unknown etiologies of ALF. For patients with features suggestive of HSV or zoster as the etiology of their ALF, empiric treatment with IV acyclovir is recommended. For patients with Hepatitis B, entecavir or tenofovir is recommended. For patients with ALF due to ischemia, such as those with Budd-Chiari syndrome, procedures aimed at restoration of blood flow are indicated.
Liver support systems, such as molecular absorbent recycling systems (MARS), have not shown to improve survival benefit in randomized controlled clinical trials.6 These artificial liver replacement systems are primarily a bridge to transplant, not a definitive intervention. There are two primary methods of treatment: cell-based therapy versus dialysis-based therapy.3 Neither cell-based therapies nor dialysis- based therapies have shown to demonstrate survival benefit.3 Evidence suggests renal replacement strategies are superior to artificial liver support, specifically CRRT. Massive renal vasoconstriction may occur in ALF patients, resulting in kidney failure from hepatorenal syndrome.2 This syndrome is only
definitively managed by liver transplant, emphasizing the need to transfer patients with ALF early to a center with transplant capabilities.
Transplant
Spontaneous survival of ALF patients is poor.2 Survival has been associated with degree of encephalopathy, with grade 3 hepatic encephalopathy patients experiencing spontaneous recovery in 40% of cases, and those with grade 4 hepatic encephalopathy having a recovery rate less than half that.3 Those who do not recover spontaneously will require a liver transplant if they are a candidate.
Since liver transplantation is so resource intensive, stratification of ALF patients is essential. For acetaminophen-associated ALF, the King’s College Criteria is used. For non-acetaminophen related ALF, the Model for End-Stage Liver Disease (MELD) system more accurately predicts in-hospital mortality.2 Although no studies explicitly validate the importance of time to transplant, the specificity of the King’s criterion, which stratifies patients by time, is up to 95% in acetaminophen induced ALF.2,10
Encephalopathy, patient age, and cause of hepatic injury are the most important survival predictors in ALF to determine probability of spontaneous recovery which occurs in <25% of patients.11 Notably, transplant outcomes continue to improve: one year survival in pediatric and adult patients are 90% and 88% respectively.
Summary
Patients presenting with altered level of consciousness, jaundice, transaminitis, and coagulopathy should raise clinical suspicion for ALF. Ruling out chronic liver disease should take precedence by taking a through history, an extensive laboratory workup including viral, autoimmune and metabolic panels.
Patients with lethargy or disorientation should be transferred to the ICU, and patients with somnolence should be intubated. All patients with concern for ALF should be risk stratified using appropriate criteria and should be considered for transfer to a transplant center. While temporizing measures including MARS devices have some clinical utility, there is no data to suggest improved survival outcome. All patients with ALF from acetaminophen should be treated with NAC. Those who do spontaneously survive ALF without transplant were nearly universally received NAC. Transplant outcomes continue to improve, with one year survival in transplant patients exceeding 90% in pediatric patients and 88% in adult patients.
1 Bernal W, Auzinger G, Dhawan A, et al. Acute liver failure. Lancet 2010;376(9736):190–201.
2 Shingina A, Mukhtar Nizar, Wakim-Fleming J, et al. Acute Liver Failure Guidelines. Am J Gastroenterol 2023; 118(7):p 1128-1153 DOI: 10.14309/ajg.0000000000002340
3 Castaldo ET, Chari RS. Liver transplantation for acute hepatic failure. HPB (Oxford). 2006;8(1):29-34. doi:10.1080/13651820500465741
4 Bajaj JS, Lauridsen M, Tapper EB, et al. Important unresolved questions in the management of Hepatic Encephalopathy: An ISHEN consensus. Am J Gastroenterol 2020;115(7):989–1002.
5 Vijay P, Lal BB, Sood V, et. al. Dynamic Optic Nerve Sheath Diameter (ONSD) guided management of raised intracranial pressure in pediatric acute liver failure. Hepatol Int. 2021;15(2):502-509. doi:10.1007/s12072-021-10139-0
6 Warrillow S, Bellomo R. Intensive Care Management of Severe Acute Liver Failure. Annual Update in Intensive Care and Emergency Medicine 2015. 2015;2015:415-430. doi:10.1007/978-3-319-13761-2_30
7 Clemmesen JO, Larsen FS, Kondrup J, et al. Cerebral herniation in patients with acute liver failure is correlated with arterial ammonia concentration. Hepatology 1999;29(3):648–53.
8 Kim YK, Seo H, Yu J, et. al. Noninvasive estimation of raised intracranial pressure using ocular ultrasonography in liver transplant recipients with acute liver failure: a report of two cases. Korean J Anesthesiol. 2013;64(5):4515. https://doi.org.ezproxy2.library.arizona.edu/10.4097/kjae.2013.64.5.451.
9 Rajajee V, Williamson CA, Fontana RJ, et. al. Noninvasive Intracranial Pressure Assessment in Acute Liver Failure. Neurocrit Care. 2018;29(2):280-290. doi:10.1007/s12028-018-0540-x
10 O’Grady JG. Transplant in Haste, repent at your leisure. Liver Transplantation. 2015. 21:5. 570-571
11 Akamatsu N, Sugawara Y, Kokudo N. Acute liver failure and liver transplantation. Intractable Rare Dis Res. 2013;2(3):77-87. doi:10.5582/irdr.2013.v2.3.77