Adapting the RUSH Protocol for Pediatrics
Brittani Campelo, DO, Vicky Kuo, MD
Alexander Arroyo, MD
Maimonides Medical Center Brooklyn NY
The Rapid Ultrasound in SHock, or RUSH protocol is used to assess the hemodynamic status and potential causes in a shock state in emergency medicine and critical care. Other protocols such as the HI-MAP protocol (Heart, IVC, Morison’s pouch, Aorta, Pulmonary), have been developed that scan similar anatomy. The utility of these protocols in pediatric shock continue to be evaluated with positive results. In this review article we will modify the RUSH protocol to better suit pathology and physiology in the pediatric patient.
The RUSH exam is useful for assessing the patient with undifferentiated shock, as well as the body’s physiologic response to treatments rendered. Shock is an acute syndrome that occurs due to cardiovascular dysfunction and the inability of the circulatory system to provide adequate oxygen and nutrients to meet the metabolic demand of vital organs (Shaw KN, Bachur RG, Chamberlain JM, et al. Fleisher & Ludwig’s Textbook of Pediatric Emergency Medicine. Lippincott Williams & Wilkins; 2016.) Shock can be divided into four categories: hypovolemic, cardiogenic, distributive, and obstructive. Hypovolemic shock stems from hemorrhage or loss of other physiologic fluid. Cardiogenic shock may be secondary to numerous forms of cardiac failure. Distributive shock encompasses the processes of sepsis, anaphylaxis, and neurologic injury, while obstructive shock includes the entities of pericardial tamponade, large pulmonary emboli, or tension pneumothorax.
Studies involving adult patients in shock in emergency medicine and critical care settings have demonstrated improved diagnostic ability and outcomes by using the RUSH protocol. A prospective observational study by Shokoohi et al concluded that early use of the RUSH protocol in patients with hypotension accurately guided diagnosis, reduced diagnostic uncertainty, and substantially improved management and resource utilization in the emergency department. An additional observational prospective study by Zieleskiewicz et.al suggested that a protocolized use of the RUSH exam for patients on the inpatient wards may improve diagnosis, time to initial treatment, and survivability of patients with developing acute respiratory or circulatory failure.
The RUSH protocol evaluates three distinct entities; the pump (heart), the tank (volume status), and the pipes (vascular integrity), though we will further sub-categorize them in consideration for the pediatric patient.
THE PUMP
Shock in children generally starts in a compensated state. Cardiac function is usually the first physiological process affected due to differences in pediatric cardiac output as compared to adults. Cardiac output in children is more dependent on heart rate than stroke volume due to a smaller left ventricular muscle mass and lower myocardial elasticity. Therefore, the first stage of shock is often demonstrated through increasing tachycardia which, if left untreated, progresses to tachycardia causing decreased diastolic filling time and a further decrease in cardiac output. Of note, blood pressure is often maintained in pediatric patients, therefore it is a poor early indicator of pediatric shock.
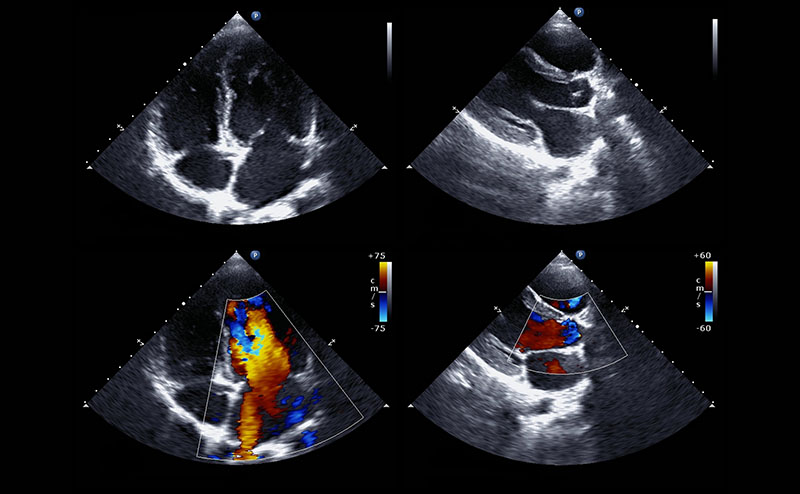
The “pump” or the heart is the first step in evaluating the undifferentiated pediatric patient in shock and their response to treatments rendered. It is evaluated in the four traditional cardiac views - parasternal long and short, subxiphoid, and apical 4 chamber. These views evaluate for pericardial effusion (including tamponade physiology), contractility, chamber dilation and sufficient filling. Decreased left ventricular (LV) contractility can indicate cardiogenic failure. Decreased LV filling can indicate problems with venous return such as obstruction of right heart blood flow or hypovolemia. Right ventricular (RV) strain or dilation may indicate pulmonary embolism. A decrease in RV filling suggests blood loss or potential neurogenic or infectious causes requiring pharmacological intervention with vasopressors or inotropes. A pericardial effusion can be assessed for tamponade physiology, and ultrasound guidance can be used to perform pericardiocentesis as indicated. Global heart dilation and or poor “squeeze” can be seen in myocarditis.
Case 1
16 year old male was a driver in a high speed motor vehicle accident. Airbags were deployed and there was a prolonged extraction time.
VS: HR 150 BP 78/46 T 97 P02 94%
General: GCS 10, Multiple facial lacerations
Cardiac: tachycardic, muffled heart sounds poor peripheral pulses
Chest: decreased breath sounds with bruising along the sternum
Abdomen: soft, but tender
Extremities: open right tibia/fibula fracture
This clip displays cardiac tamponade with a large pericardial effusion. The effusion is causing diastolic collapse of the right ventricle and is concerning for tamponade physiology.
Case 2
3 month old male with 4 days of fever, respiratory distress, poor feeding
VS: HR 80 BP 60/palp T 97 P02 84%
General: Pale, lethargic, minimally responsive
Cardiac: Tachycardic, murmur, thready brachial pulse
Chest: Respiratory distress with diffuse crackles
This video displays severe LV dilatation and systolic dysfunction with moderate inferior pericardial effusion. The patient ultimately was diagnosed with Anomalous Left Coronary Artery from the Pulmonary Artery (ALCAPA). In this process, the left coronary artery (LCA) arises from the pulmonary artery instead of the aorta, leading to a reversed blood flow and reduced oxygen supply to the heart muscle, causing ischemia and potentially heart failure.
Case 3
7 month old female with 1 day of sweating with feeds, shortness of breath, crankiness and decreased oral intake.
VS: HR 230 BP 70/40 T 98 P02 95%
General: Pale, crying
Cardiac: Tachy, no murmur
Chest: Clear
EKG: narrow complex tachycardia with no discernible P waves
This patient is in SVT and has received a dose of adenosine, you can see the heart rate decrease to normal post adenosine therapy.
THE TANK
The “tank,” or the vascular and extravascular volume, can be assessed for fullness, leakiness, or compromise.
Tank Fullness:
This can be evaluated at the inferior vena cava. Of note, studies regarding the validity of IVC (inferior vena cava) to aorta (Ao) ratio for the evaluation of dehydration and fluid responsiveness in pediatric patients are conflicting, as opposed to adult studies where the measurements are validated. The IVC is measured in the longitudinal axis during exhalation and the aorta is measured in longitudinal during systole. In adults, a normal IVC/Ao ratios are between 0.8-1.2. A ratio below 0.8 suggests dehydration and one above 1.2 suggests overload.
A plethoric IVC with little respiratory variation is concerning for right-sided heart overload, strain or hypervolemia. Poor LV function in the setting of an enlarged, non-collapsible IVC is highly suggestive of cardiogenic shock. An IVC that collapses more than 50% with inspiration is concerning for hypovolemia.
Extravascular volume can be evaluated in the intestines to gauge if a patient has or will have potential ongoing losses by visualizing large amounts of fluid in the intestinal system.
Of note, several case reports have postulated the utility of the addition of intracranial ultrasound for infants with an open anterior fontanelle to evaluate for intracranial hemorrhage, hydrocephalus, and infections which can all be causes of undifferentiated hypotension and shock. In order to perform this exam the transducer is placed over the anterior fontanelle in the coronal and sagittal orientation with the goal to visualize the superior sagittal sinus for midline orientation followed by the superficial surface of the brain for extra axial fluid. Increasing the depth of the view can also show ventricular size which if enlarged, may be an indicator of hydrocephalus.
Case 4
18 month old female with 4 days of fever, vomiting, copious diarrhea and no urine output
VS: HR 180 BP 60/palp T 97 P02 93%
General: Pale, lethargic, not responsive
Cardiac: Tachy, thready brachial pulse
Chest: Normal breath sounds
Skin: Dry and tenting
Bowel ultrasound showing a large amount of intraluminal fluid representing ongoing losses from diarrhea.
A flat, slit-like IVC is seen with little respiratory variation.
Tank Leakiness:
POCUS can determine the presence of extravascular fluid in the thoracic, abdominal, or pelvic compartments. Examples of some entities that might present with shock and free fluid include traumatic abdominal organ rupture or ruptured ectopic pregnancy. The cardiac and pulmonary portions of the FAST are covered in different sections. The intestines are evaluated for signs of bowel obstruction by using a window box technique in which scanning starts in the right upper quadrant and moves to the left upper, left lower and right lower, obtaining transverse and longitudinal images in each section. A dilated small bowel loop measuring more than 2.5-3.0 cm in diameter strongly suggests bowel obstruction or ileus.
An edematous bowel wall measuring more than 3 mm may indicate obstruction or an inflammatory process. Entities that may be encountered are a ringed mass with or without sufficient color flow (intussusception), lack of peristalsis with to-and-fro movement of intestinal contents (obstruction, ileus), dilated thick bowel (infection, injury, obstruction), free fluid (perforation, inflammation) or air in the abdominal cavity which may present as reverberating A-lines that is normally seen in the lung (intestinal or diaphragmatic perforation).
Case 5
8 year old male with a past surgical history of appendectomy 1 year ago presents with abdominal pain and vomiting for 2 days
VS: HR 160 BP 65/46 T 99 RR 40 P02 99%
General: pale and ill appearing
Cardiac: tachycardic with no murmur
Abdomen: rigid, tender to palpation
Small bowel is dilated with to-and-fro movement of intestinal contents representing obstruction. Visualization of the finger-like plicae circulares (“keyboard sign”) is also appreciated.
Bowel wall thickened representing obstruction in a patient with adhesions after surgery.
Case 6
15 year old male with high impact trauma to abdomen after skateboarding at the indoor park
VS: HR 145 BP 80/63 T 98 P02 95%
General: Pale and diaphoretic, clutching abdomen
Cardiac: Tachy
Chest: Clear to auscultation bilaterally
Abdomen: Bruised, distended, tympanitic and tender
Multiple reverberating A-lines are seen in the abdomen of this patient obscuring the abdominal contents representing free air from an intestinal rupture.
The same patient - now the liver and gallbladder are seen to the left of the image with the A-lines on the right side.
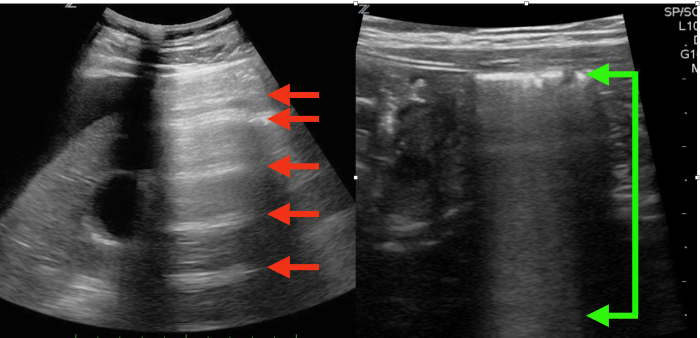
The left image red arrows shows reverberating horizontal A lines in the abdomen indicating free air from a ruptured viscus, the right image green arrows shows how normal bowel gas appears.
Tank Compromise:
The thoracic cavity is a ‘tank’ and may be assessed by evaluating bilateral upper and lower lung fields to assess for pneumothorax and pneumonia (B lines, consolidation, spine sign).
Lack of sliding with a classic barcode sign on M-mode can be suggestive of pneumothorax in the correct clinical picture. At times a lung point, the transition point between normal pleura and pneumothorax, can be seen as a drop off of motion on the pleura.
In healthy lung, air causes poor transmission of ultrasound beams, and underlying structures are not able to be visualized directly. Consolidations, such as pneumonia, allow the operator to see structures inside the lung. Finally, B-lines, bright white lines extending down from the pleura, suggests fluid overload.
Case 7:
15 year old male with shortness of breath and chest pain after gym class, past medical history of “some heart thing” per mother
VS: HR 130 BP 90/60 T 99 RR 55 P02 88%
General: Tall, thin, anxious, nasal flaring, SOB
Lungs: Decreased breath sounds left lung all fields, right clear to auscultation
Cardiac: Left-sided JVD, distant heart sounds
A pneumothorax is seen in the left lung. To the left of the screen you can see the pleura shimmering/moving. To the right the pleura is not moving. The transition point is called ‘lung point.’ An M mode spike shows the “waves on the beach” appearance of the normal pleura on the left and “bar code” sign on the right representing pneumothorax.
Case 8:
4 year old female with 5 days of fever, severe cough and decreased oral intake
VS: HR 160 BP 70/45 T 105.5 P02 90%
General: pale, lethargic, toxic appearing
Cardiac: tachy, thready pulses
Lungs: decreased breath sounds right side with rales
A large lung consolidation is seen to the left of the image above the diaphragm. The spine is seen below this consolidation (spine sign) when in a healthy lung the spine is obscured due to the impedance air has on ultrasound beams.
The same patient with the consolidation on the lower portion of the screen again displaying spine sign.
THE PIPES
This evaluates the femoral and popliteal vessels for DVT, and the aorta for trauma, aneurysms or dissection. DVT should be evaluated starting at the branching point of the common femoral vein and traced down behind the knee to the popliteal vein using graded compression to ensure collapsibility of the vein. Although extremely rare in children, the aorta can be evaluated for injury, aneurysm and dissection. The aorta may be visualized in 4 regions including the suprasternal, parasternal, epigastric, and supraumbilical aorta.
Case 9:
11 year old female with cerebral palsy and seizure disorder, wheelchair bound, presents with
progressive shortness of breath
VS: HR 170 BP 80/56 T 102.4 RR 46 P02 90%
General: Pale and ill appearing, shortness of breath, nasal flaring
Lungs: Coarse breath sounds bilaterally
Cardiac: Tachycardic no murmur
Extremities: Swollen, tender, red left calf and lower thigh
A thrombus is seen in the common femoral vein and does not change with compression. Color flow demonstrates arterial flow in the femoral arteries and absent flow in the femoral vein.
Cited sources:
Shaw KN, Bachur RG, Chamberlain JM, et al. Fleisher & Ludwig’s Textbook of Pediatric Emergency Medicine. Lippincott Williams & Wilkins; 2016. Accessed February 18, 2025. https://emergency.lwwhealthlibrary.com/book.aspx?bookid=1692&sectionid=0
Shokoohi H, Boniface KS, Pourmand A, Liu YT, Davison DL, Hawkins KD, Buhumaid RE, Salimian M, Yadav K. Bedside Ultrasound Reduces Diagnostic Uncertainty and Guides Resuscitation in Patients With Undifferentiated Hypotension. Crit Care Med. 2015 Dec;43(12):2562-9. doi: 10.1097/CCM.0000000000001285. PMID: 26575653.
Zieleskiewicz L, Bouvet L, Einav S, Duclos G, Leone M. Diagnostic point-of-care ultrasound: applications in obstetric anaesthetic management. Anaesthesia. 2018 Oct;73(10):1265-1279. doi: 10.1111/anae.14354. Epub 2018 Jul 26. PMID: 30047997.
Additional Resources:
Ghane MR, Gharib MH, Ebrahimi A, Samimi K, Rezaee M, Rasouli HR, Kazemi HM. Accuracy of Rapid Ultrasound in Shock (RUSH) Exam for Diagnosis of Shock in Critically Ill Patients. Trauma Mon. 2015 Feb;20(1):e20095. Doi: 10.5812/traumamon.20095. Epub 2015 Feb 20. PMID: 25825696; PMCID:PMC4362031.
Hardwick JA, Griksaitis MJ. Fifteen-minute consultation: Point of care ultrasound in the management of paediatric shock. Arch Dis Child Educ Pract Ed. 2021 Jun;106(3):136-141. doi: 10.1136/archdischild-2019-317972. Epub 2020 Aug 7. PMID: 32769083.
Keikha M, Salehi-Marzijarani M, Soldoozi Nejat R, Sheikh Motahar Vahedi H, Mirrezaie SM. Diagnostic Accuracy of Rapid Ultrasound in Shock (RUSH) Exam; A Systematic Review and Meta-analysis. Bull Emerg Trauma. 2018 Oct;6(4):271-278. doi:10.29252/beat-060402. PMID: 30402514; PMCID: PMC6215077.
Musolino AM, Buonsenso D, Massolo AC, Gallo M, Supino MC, Boccuzzi E. Point of care ultrasound in the paediatric acute care setting: Getting to the heart of respiratory distress. J Paediatr Child Health. 2021 Mar;57(3):318-322. doi: 10.1111/jpc.15308. Epub 2020 Dec 9. PMID: 33295654.
Octavius GS, Imanuelly M, Wibowo J, Heryadi NK, Widjaja M. Inferior vena cava to aorta ratio in dehydrated pediatric patients: a systematic review and meta-analysis. Clin Exp Pediatr. 2023 Nov;66(11):477-484. doi: 10.3345/cep.2022.01445. Epub 2023 Jun 14. PMID: 37321576; PMCID: PMC10626024.
Perera P, Mailhot T, Riley D, Mandavia D. The RUSH exam: Rapid Ultrasound in Shock in the evaluation of the critically lll. Emerg Med Clin North Am. 2010 Feb;28(1):29-56, vii. doi: 10.1016/j.emc.2009.09.010. PMID: 19945597.