My, Oh My, It’s an MI! A Clinical Case Demonstrating the Utility of the Transgastric Short Axis View in Resuscitative TEE
Zackary Funk, MD
Jordan Tozer, MD
Virginia Commonwealth University
Case Presentation
EMS calls prehospital report with a 60-year-old male who had a witnessed arrest after complaining of chest pain. Bystander CPR was initiated. The patient was pulseless on EMS arrival and ventricular tachycardia was observed upon placement of the defibrillator pads. EMS delivered two shocks, an ET tube was placed with good capnography, and one ampule of epinephrine was administered en route—the total time since collapse was estimated at 15 minutes prior to arrival in the ED.
Background
Point-of-care application of focused transesophageal echocardiography (TEE) in cardiac arrest and the resuscitation of critically ill patients can provide clinicians with insights into the presence of reversible pathologies.1-3 The transgastric-midpapillary short axis (TG SAX) view can be used to assess for evidence of myocardial ischemia/infarction as a potential etiology leading to cardiac arrest and profound shock states.2
Compared to the transthoracic approach, TEE can offer superior image quality and circumvent practical limitations such as the inability to obtain adequate views from either patient factors such as body habitus, bowel gas, and other anatomic challenges and constraints posed by the need for chest compressions, defibrillation pads, and resuscitative efforts.3
The American Heart Association recognizes a 17-segment model of the left ventricle to describe distinct areas of potential regional abnormalities based on vascular territories. While useful in the detailed assessment of manifestations of coronary artery disease and malperfusion, the cumbersome nature of the assessment and knowledge required in its application is somewhat prohibitive in the rapidly evolving and time-sensitive resuscitation phase of patient care.4,5
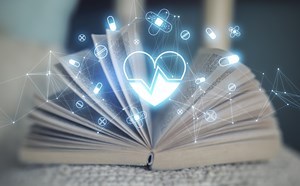
In the focused approach utilized in resuscitative TEE, evaluation of regional wall motion abnormalities in the major vascular territories of the left anterior descending (LAD), left circumflex (LCx), and right coronary artery (RCA) can be performed using the TG SAX view at the level of the midpapillary plane. To obtain this view, the operator will advance the TEE probe to an approximate depth of 40cm from the incisors, set the omniplane angle between 0-20 degrees, and anteflex the probe sufficiently to obtain the view demonstrated in Figure 1 and Figure 2. With slight adjustments in the depth of insertion further assessment of the base and apex of the left ventricle can be obtained.
 Figure 1. Diagram of the anatomy evaluated using the TGSAX view. Graphic courtesy of ACEP EUS Critical Care Subcommittee.
Figure 1. Diagram of the anatomy evaluated using the TGSAX view. Graphic courtesy of ACEP EUS Critical Care Subcommittee.
 Figure 2. Transgastric midpapillary view demonstrating the left ventricle and papillary muscles visualized at approximately 40cm depth from the incisions, omniplane between 0-20 degrees, and anteflexion of the probe. This patient demonstrates global left ventricular hypokinesis. Image courtesy of Lindsay Taylor, MD.
Figure 2. Transgastric midpapillary view demonstrating the left ventricle and papillary muscles visualized at approximately 40cm depth from the incisions, omniplane between 0-20 degrees, and anteflexion of the probe. This patient demonstrates global left ventricular hypokinesis. Image courtesy of Lindsay Taylor, MD.
Hypokinesis or akinesis of the left ventricular myocardium segments can indicate tissue ischemia or infarction in specific vascular territories (Figures 3a and 3b). The RCA supplies the myocardium of the inferior wall of the left ventricle. On TEE, the inferior wall is located closest to the probe footprint, since the probe is coming from the stomach located inferior to the heart. The LAD supplies the myocardium of the anterior and septal portions of the left ventricle. The circumflex artery supplies the lateral portion of the left ventricular myocardium and will be shown on the rightward aspect of the ultrasound image.4
In the absence of regional wall motion abnormalities or other confounding factors, the operator should observe the left ventricle walls concentrically and symmetrically contracting toward the center-most aspect of the left ventricle cavity during ventricular systole. Any asymmetry during this process should raise concerns about a wall motion abnormality in one of the distributions noted above and, thereby, concerns of myocardial ischemia/infarction.
 Figure 3a. Walls of the left ventricle as seen on TGSAX with vascular territories. The left ventricle here demonstrates global hypokinesis rather than pathology isolated to one vascular territory. Image courtesy of Lindsay Taylor, MD.
Figure 3a. Walls of the left ventricle as seen on TGSAX with vascular territories. The left ventricle here demonstrates global hypokinesis rather than pathology isolated to one vascular territory. Image courtesy of Lindsay Taylor, MD.
 Figure 3b. The septal wall exhibits focal akinesis (arrow) in addition to global hypokinesis which may suggest an acute LAD lesion in the right clinical context. Image courtesy of Lindsay Taylor, MD.
Figure 3b. The septal wall exhibits focal akinesis (arrow) in addition to global hypokinesis which may suggest an acute LAD lesion in the right clinical context. Image courtesy of Lindsay Taylor, MD.
Case Resolution
The patient complained of chest pain just before their arrest and suffered recurrent ventricular dysrhythmia, suggestive of myocardial ischemia as a potential underlying etiology. Prolonged periods of sustained ROSC between dysrhythmias were not achievable, preventing ECG analysis. However, evaluation of the myocardium using TEE was feasible. The TG SAX view revealed a focal region of poor contractility in the anterior wall, supporting the suspicion of ischemia and localizing the distribution to the LAD.
With this information and favorable patient factors, including prompt bystander CPR and relatively short downtime, systemic thrombolytics were administered, and continuous mechanical CPR was performed per protocol. A rhythm check was performed at 30 minutes post-thrombolytic administration. He demonstrated an accelerated idioventricular rhythm (AIVR) on ECG with a palpable pulse and improved contractility observed on the TEE assessment compared to the pre-intervention assessment.
The patient was subsequently admitted to the cardiac intensive care unit, and follow-up left heart catheterization revealed significant disease of the proximal LAD. He underwent stent placement and was able to be successfully discharged to a cardiac rehab facility thereafter.
Summary
Regional wall motion abnormalities in the peri-arrest patient can be detected using the transgastric short-axis view during resuscitative transesophageal echo evaluation. The presence of these findings can provide evidence to suggest acute myocardial ischemia/infarction as the underlying etiology of a patient’s arrest or shock state and guide the use of potentially life-saving interventions such as systemic thrombolysis. Familiarity with the techniques for detecting these findings can arm clinicians to tailor and target their resuscitation of critically ill patients.
References
- Fair J, Mallin M, Mallemat H, et al. Transesophageal echocardiography: guidelines for point-of-care applications in cardiac arrest resuscitation. Ann Emerg Med. 2018;71(2):201-7.
- McGuire D, Johnson S, Mielke N, Bahl A. Transesophageal echocardiography in the emergency department: a comprehensive guide for acquisition, implementation, and quality assurance. J Am Coll Emerg Physicians Open. 2022;3(3):e12758.
- Teran F, Dean AJ, Centeno C, et al. Evaluation of out-of-hospital cardiac arrest using transesophageal echocardiography in the emergency department. 2019;137:140-7.
- Cerqueira MD, Weissman NJ, Dilsizian V, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: a statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. 2002;105(4):539-42.
Reeves ST, Finley AC, Skubas NJ, et al. Basic perioperative transesophageal echocardiography examination: a consensus statement of the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. J Am Soc Echocardiogr. 2013;26(5):443-456.