Rapid Recognition of Testicular Torsion on Bedside POCUS
Trenton Rivera, MD
Nicklaus Children’s Hospital PEM Fellow
Paul Khalil, MD
Nicklaus Children’s Hospital POCUS Fellowship Program Director
A 12-year-old male presents to your emergency department with testicular pain. The pain has been present for 3 hours and it “came out of the blue” without a history of trauma. He has no past medical history. However, upon further questioning, he reports that this same pain occurred last week for a short period of time and then went away. The patient was embarrassed and did not tell anyone. On exam, the right testicle is high-riding and swollen. The patient is writhing in pain and eliciting a cremasteric reflex is difficult. Other than being tachycardic and hypertensive from pain, his vital signs are within normal limits, and he has no recent upper respiratory infection symptoms. Due to your high clinical concern for testicular torsion, you decide to use POCUS to help differentiate the cause of his testicular pain. Remembering that a torsed testicle will lack blood flow, you use color Doppler during your exam.
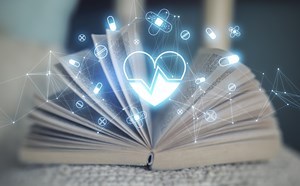
 Image 1. Color Doppler of a testicle without blood flow to the body of the testicle concerning for testicular torsion.
Image 1. Color Doppler of a testicle without blood flow to the body of the testicle concerning for testicular torsion.
[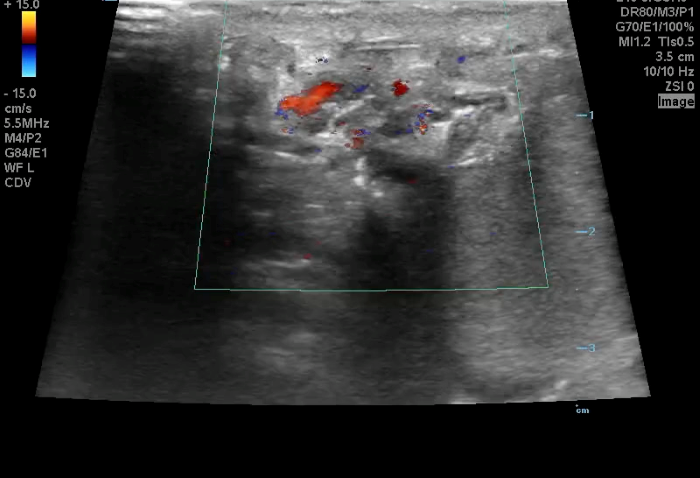 Image 2. Twisted spermatic cord (“corkscrew sign”) concerning for testicular torsion.
Image 2. Twisted spermatic cord (“corkscrew sign”) concerning for testicular torsion.
In your first image (Image 1), you realize there is no flow with color Doppler. Additionally, you find a torsed cord complex (Image 2), also known as the “corkscrew sign.” You consult Urology who is busy in the operating room with another case. You decide to perform a manual detorsion due to your concern for testicular atrophy and risk of infertility. Using the open book technique, you get relief of pain and return of vertical positioning of the testicle after two rotations. On your repeat testicular POCUS with color Doppler you obtain these images (Images 3 and 4), which demonstrate venous and arterial flow throughout the testicle. The cord is now untwisted and appears linear in orientation.
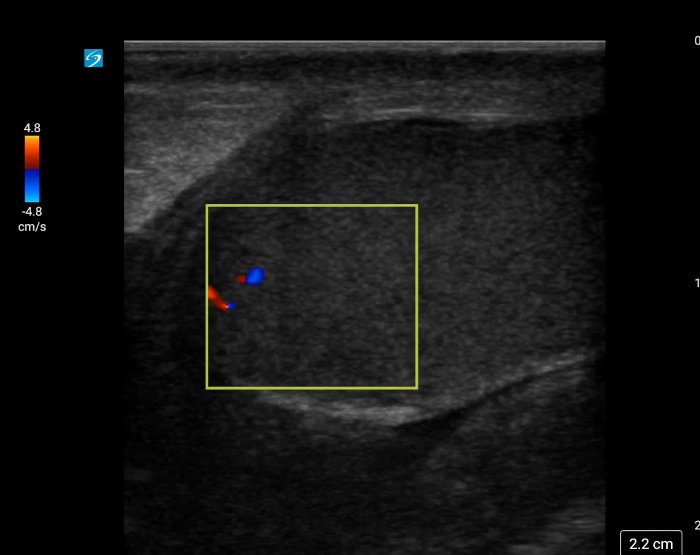 Image 3. Color Doppler demonstrating intratesticular flow toward and away from the probe.
Image 3. Color Doppler demonstrating intratesticular flow toward and away from the probe.
 Image 4. Linear, untwisted appearance of the spermatic cord with accompanying vessels.
Image 4. Linear, untwisted appearance of the spermatic cord with accompanying vessels.
Due to your ability to rapidly diagnose testicular torsion on POCUS with color Doppler, you were able to return blood flow to the patient’s testicle before the surgeon, or the operating room, was available. The patient subsequently undergoes an uncomplicated orchiopexy and is discharged home the same day.
Background
Testicular torsion is a relatively common cause of scrotal pain in children with an incidence of 1 in 4000 by the age of 25.1 Testicular torsion is an urologic emergency due to the risk of lost fertility following ischemic injury to the testicle.2 Earlier return of blood flow has been shown to increase likelihood of testicular salvage.3 Ultrasound (US) using color Doppler is the preferred way to determine if testicular torsion is present in indeterminate cases of testicular pain.4 As point-of-care ultrasound becomes more available and more widely taught, emergency medicine physicians have a unique opportunity to make rapid diagnoses, expediting care of a surgical emergency.
Historically, Doppler ultrasonography has a sensitivity of 88.9% and a specificity of 98.8% with a false-negative rate of 1%.5 In the case of testicular torsion, color Doppler will show reduced or absent blood flow of the affected testicle. Scanning the spermatic cord for corkscrew sign (twisted appearance), increases the accuracy of POCUS in partial or incomplete torsion.6
Technique
The high frequency linear probe (10-15 MHz) is used for testicular POCUS as it provides for a large footprint for a superficial area of interest just below the scrotal skin.7 Ultrasound with color Doppler is useful to appreciate direction of blood flow and is the preferred method for detecting blood flow in the testicle when assessing for testicular torsion. Power Doppler, which detects the integrated power of the Doppler signal, has an increased sensitivity for detecting blood flow when there is a low flow state, such as in prepubertal males and partial testicular torsion. If there is suspicion for low residual flow, lowering the pulse repetition frequency (PRF) can assist in detecting smaller pulse waveforms.8 However, this increased sensitivity also detects motion artifact, which can be falsely reassuring.8 Adjust your settings when scanning the unaffected testicle before scanning the affected testicle.
Position
The patient should be placed in a supine position with the scrotum being supported by a towel and the penis held out of the field of view. (Image 5) This can be done by placing the penis cranially on the abdomen and placing a towel on top of the penis. Use a copious amount of gel to reduce pain and improve acoustic coupling. Pain medication may be needed to complete a thorough testicular POCUS exam.7
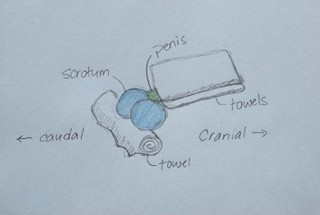 Image 5. Cartoon illustration of patient positioning for testicular POCUS.
Image 5. Cartoon illustration of patient positioning for testicular POCUS.
Sequence of scanning:
View 1: Side by side (Buddy View)
Place the linear probe in transverse orientation across both testicles. This allows you to quickly visualize the echogenicity, size, blood flow and position of both testicles in one view. It also allows for your first opportunity of comparison between the two testicles.
Video 1. Buddy view of both testicles side-by-side.
View 2: The Unaffected Testicle
Using greyscale, scan the unaffected testicle in both longitudinal and short axes. Use color Doppler to assess for blood flow. Be sure to set your preferred gain and color Doppler settings on the unaffected testicle to allow for comparison to the affected testicle.
- A healthy testicle should appear oval-shaped and roughly 3–5 cm in length, by 2–3 cm in width depending on the age. Testicles have a homogeneous appearance with a medium-level echogenicity (like other solid organs). They are smooth and uniform throughout when healthy. Start by fanning through the testicle in transverse and longitudinal orientations to get a general assessment. When applying color Doppler to a well perfused testicle, there should be uniform, low velocity arterial and venous blood flow throughout the parenchyma. Vessels may appear pinpoint, linear or branching. Using spectral Doppler, the velocity of specific vessels can be measured. Arterial flow will appear as a brisk upstroke and sharp downstroke reflecting the cardiac cycle. Venous flow has a continuous velocity with less variation, often described as a “venous hum” (Images 6 and 7).7
Video 2. Fanning through a normal testicle.
Video 3. Color Doppler pulsations indicating blood flow within the body of the testicle.
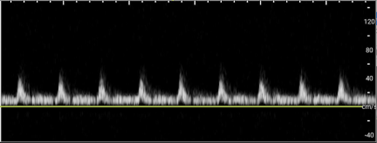 Image 6. Arterial flow on Spectral Doppler.
Image 6. Arterial flow on Spectral Doppler.
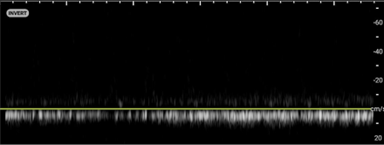 Image 7. Venous flow on Spectral Doppler.
Image 7. Venous flow on Spectral Doppler.
View 3. The Affected Testicle
Similar to the unaffected testicle, start in greyscale with views in the long and short axis. While examining, compare the echogenicity, size and positioning. Be on the lookout for masses, cysts or hydroceles that could also present with scrotal pain. Then proceed to scanning the testicle and spermatic cord with color Doppler.
- A testicle affected by torsion may appear larger due to swelling in the early stages. In the later stages, the testicle may appear atrophic with heterogenous echogenicity, due to ischemia, and may also contain a reactive hydrocele which appears as a hypoechoic fluid pocket around the testicle. (Video 4 and 5) Using color Doppler, you will see absent or significantly reduced blood flow to the body of the affected testicle. When unclear, compare to the unaffected side to appreciate a reduction in blood flow. You may try increasing the color with color Doppler to ensure there is no flow to the testicle.9
- In addition to qualitatively assessing blood flow in the testicle, you may also use spectral Doppler to calculate a Resistive Index. Positioning the gate over the testicular artery and utilizing pulse-wave Spectral Doppler will allow you to quantify the resistance within the vessel. Most machines will automatically do this calculation if prompted, however the resistive index can also be calculated using the following equation:
RI = (Peak Systolic Velocity – End Diastolic Velocity) / Peak Systolic Velocity
A normal RI for a well perfused testicular is 0.5-0.7. If the RI is > 0.7, it suggests that there is an increase in the resistance to flow concerning for partial or early testicular torsion.10
Video 4. Greyscale view demonstrating a torsed testicle with heterogeneous echogenicity (infarct) and a reactive hydrocele.
Video 5. Atrophic testicle with heterogenous echogenicity and large reactive hydrocele due to prolonged torsion.
The Cord
The spermatic cord can be found at the superior pole of the testicles. Although included in this article after the affected testicle, it should be scanned after each testicle. The normal spermatic cord should have a linear appearance with an accompanying vessel demonstrating blood flow with color Doppler.9
Video 6. Linear spermatic cord with smooth appearing vessels.
In the presence of testicular torsion, the spermatic cord will have a twisted appearance at the superior testicle. Twisting of the spermatic cord, commonly known as corkscrew sign, may be visible at the superior testis. (Image 8)
Video 7. Color Doppler demonstrating a twisted spermatic cord.
 Image 8. The corkscrew sign can be appreciated when using color Doppler.
Image 8. The corkscrew sign can be appreciated when using color Doppler.
Pitfalls
- Early or partial torsion may still have detectable blood flow. Partial torsion may present with loss of venous blood flow and retention of arterial blood flow due to pressure differences in the vessels. Ultrasound has a lower sensitivity in these cases. Lowering the PRF when using Doppler will allow for better detection in low flow states.8
- Blood flow to the capsule of the testicle can be present during testicular torsion. It is important to focus on the intratesticular (body of the testicle) blood flow to avoid false reassurance.8
- In prepubertal boys, low baseline flow can make interpretation challenging.8
- Epididymitis can mimic testicular torsion clinically but should show hyperemia or increased blood flow on US with Doppler.8
Integration into clinical practice
POCUS with Doppler should be used in the indeterminate cases of acute testicular pain. When your history and exam are consistent with or highly suspicious for testicular torsion, you should immediately consult your surgical team and facilitate getting the patient to the operating room. When time allows or the diagnosis is less clear, POCUS with Doppler can be a highly specific adjunct in the assessment of testicular torsion. Reduced or absent blood flow should immediately trigger a surgical consult. If the blood flow is present, but there is suspicion for a torsion-detorsion sequence based on history, assess the testicle greyscale looking for signs of recent ischemia or reactive hydrocele. Additionally, scan the spermatic cord for a twisted appearance (corkscrew sign) to increase your accuracy. Finally, do not let POCUS delay surgery in the highly suspicious cases of testicular torsion. POCUS should expedite cases to the operating room when the etiology is unclear by history and exam.
References
- Williamson RC. Torsion of the testis and allied conditions. Br J Surg. 1976;63:465.
- Romeo C, Impellizzeri P, Arrigo T, et al. Late hormonal function after testicular torsion. J Pediatr Surg. 2010;45:411.
- Howe AS, Vasudevan V, Kongnyuy M, et al. Degree of twisting and duration of symptoms are prognostic factors of testis salvage during episodes of testicular torsion. Transl Androl Urol. 2017;6(6):1159-1166.
- Baker LA, Sigman D, Mathews RI, Benson J, Docimo SG. An analysis of clinical outcomes using color Doppler testicular ultrasound for testicular torsion. Pediatrics. 2000;105(3 pt 1):604-607.
- Sharp VJ, Kieran K, Arlen AM. Testicular torsion: diagnosis, evaluation, and management. Am Fam Physician. 2013;88(12):835-40.
- American Institute of Ultrasound in Medicine; American College of Radiology. Practice parameter for the performance of scrotal ultrasound examinations. AIUM; 2021.
- Morgan M, Sharma R, Walizai T, et al. Testicular and scrotal ultrasound. Reference article, Radiopaedia.org (Accessed on 13 Aug 2025) https://doi.org/10.53347/rID-33262
- Bomann J. Chapter 13. Testicular Ultrasound. In: Carmody KA, Moore CL, Feller-Kopman D. eds. Handbook of Critical Care and Emergency Ultrasound. The McGraw-Hill Companies; 2011.
- Gaillard F, Weerakkody Y, Jha P, et al. Testicular torsion. Reference article, Radiopaedia.org (Accessed on 13 Aug 2025) https://doi.org/10.53347/rID-10959
- Shih J. Ultrasound For The Win: 22M with Scrotal Pain. February 12, 2015. Accessed August 13, 2025. https://www.aliem.com/ultrasound-win-22m-scrotal-pain-us4tw/