The Importance of Coverage in Emergency Ultrasound Reimbursement
Chris Thom, MD, RDMS, FPD-AEMUS
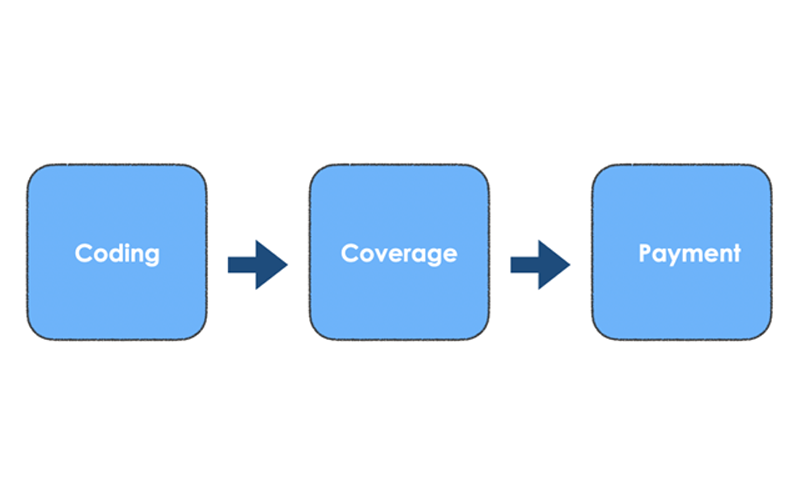
In Emergency Ultrasound (EUS) reimbursement, we often find our focus directed towards the relevant CPT codes and associated documentation requirements. However, there is a second step to successful EUS reimbursement that is just as important as the Coding process. This is broadly termed as “Coverage” and denotes the determination of whether a given payer will actually reimburse for the EUS performed. A basic understanding of this variable can improve the likelihood that your valuable work using EUS in clinical practice is appropriately reimbursed.
This language from the Section 1862(s) of the Social Security Act sums the concept up nicely: “No payment may be made under Part A or Part B for any expenses incurred for items or services not reasonable and necessary for the diagnosis or treatment of illness or injury or to improve the functioning of a malformed body member.”
In essence, coverage determinations are made by payers to assess whether a test or intervention being performed is medically necessary for the given clinical condition or diagnosis.
Medicare Coverage Determinations
Medicare provides publicly available policies regarding their coverage determination process. Coverage can be determined on a National Coverage Determination (NCD) basis or can be deferred down to local Medicare Administrative Contractors (MACs). The list of nationally covered indications pertaining to diagnostic and procedural ultrasound is found here: NCD - Ultrasound Diagnostic Procedures (220.5).1 Note that this list was last updated in 2007.
Enter the MACs
For services that are not specifically listed as being covered by Medicare or explicitly stated as being non-covered by Medicare, the local MAC can establish the relevant medical coverage policies. Interestingly enough, MACs are private companies that have been awarded a geographic jurisdiction to process medical claims. In addition, they establish Local Coverage Determinations (LCD’s), which can define whether a specific medical service is covered and under what circumstances. The list of MACs can be found here: Medicare Administrative Contractors (MACs) 03.28.2023.2
Private Payers
Coverage by private payers varies by payer, as they are given wide latitude in their coverage determinations. There is variance in what payers will consider as medically necessary and what they will consider as an experimental or investigational usage of ultrasound. For example, Aetna currently lists ultrasound guidance for lumbar puncture as a medically necessary adjunct that would allow for coverage.3 This would allow a physician to successfully get reimbursed for both a lumbar puncture and CPT 76942 (ultrasound guidance for needle placement) through Aetna. However, Aetna considers the erector spinae block for management of post-operative pain to be investigational and thus not covered.4 Private payers may also have policies where they reimburse certain ultrasound procedures only to specific types of medical specialties.
The Link to ICD-10 Codes
Coverage determinations are often made by the linkage to ICD-10 codes. Many ultrasound CPT codes will feature an associated list of ICD-10 codes that support medical necessity and thus help support coverage. By way of example, CPT 76882 is the limited nonvascular extremity ultrasound code that many of us will use for our extremity abscess versus cellulitis examinations. This code lists “cellulitis of the right lower limb” as an ICD-10 code that supports medical necessity, while not listing “redness and swelling of the ankle.”4 If one had performed an ultrasound around the ankle area and determined there was cellulitis present, the chance of coverage for CPT 76882 reimbursement would be higher if one selected the “cellulitis of right lower limb” ICD-10 code instead of “redness and swelling of the ankle.”
Signs and Symptoms Matter Too
Depending on one’s coding team and processes, symptoms documented in the provider note can also be used to support medical necessity for an EUS examination. A relevant example could be the proceeding one involving 76882 and lower extremity cellulitis versus abscess. If the HPI or MDM documented leg pain as a presenting symptom, then a coder could use that symptom diagnosis as an appropriate medical necessity for the EUS examination. This could increase the chance of coverage from a payer. Note that “pain in the right leg” is listed as an acceptable ICD-10 code for 76882.4
Case 1
A 34-year-old presented to the ED after a high speed MVC. He underwent a FAST examination with an appropriate FAST EUS report documented in the medical record. The patient received CT imaging of the Chest/Abdomen/Pelvis, which was negative aside from a single anterior rib fracture. The documentation included the presence of abdominal pain in the HPI. In this case, there is an ICD-10 code to support the limited abdominal ultrasound (CPT 76705) component of the FAST exam, but not one to support the limited echocardiographic exam (CPT 93308). The patient had noted chest pain associated with the rib fracture, but this was not documented in the HPI or as a listed diagnosis. Given this, it is unlikely the limited echo component of the FAST exam will be reimbursed.
Case 1 - Revisited
Let’s look at that same case again. This time, the provider adds the accurate documentation that the patient is having chest pain with breathing, likely resultant from the rib fracture. If that is documented, then there is now a symptom diagnosis that can be used to support 93308.5 Due to this additional documentation, there is now support for the medical necessity of both components of the FAST exam.
The Bottom Line
Coverage determinations are often complex and payer dependent. A working knowledge of the role of ICD-10 codes in supporting medical necessity can be helpful to ensure one is appropriately reimbursed for EUS examinations.
References