
Clearing the C-Collar in the Emergency Department: A Practical Guide
Author:
Sean Murphy, DO
USF Emergency Medicine-PGY2
Introduction
Cervical spine (C-spine) injuries are a critical consideration in trauma patients. Emergency department (ED) providers must balance the need to protect the spine from further injury with the goal of minimizing unnecessary immobilization, which can lead to complications such as pressure ulcers, discomfort, and increased resource utilization. This post will guide you through the evidence-based approach to clearing a cervical collar in the ED using validated clinical criteria, discuss common pitfalls, and provide clinical cases for practical application.
The Evaluation Process
1. Primary Survey & Initial Assessment
- As part of the ABC’s in trauma (Airway, Breathing, Circulation), assess for any signs of high-energy trauma that could indicate a C-spine injury.
- Maintain spinal precautions in any patient with potential C-spine injury until clearance is confirmed.
- Identify red flags such as:
- Midline neck pain or tenderness
- Focal neurological deficits (e.g., weakness, paresthesia)
- Altered mental status or intoxication
- Significant distracting injuries
2. Clinical Decision Rules for Clearing the C-Spine
In the emergency department there are two widely used, evidence-based clinical decision tools to help determine if imaging is necessary before collar removal:
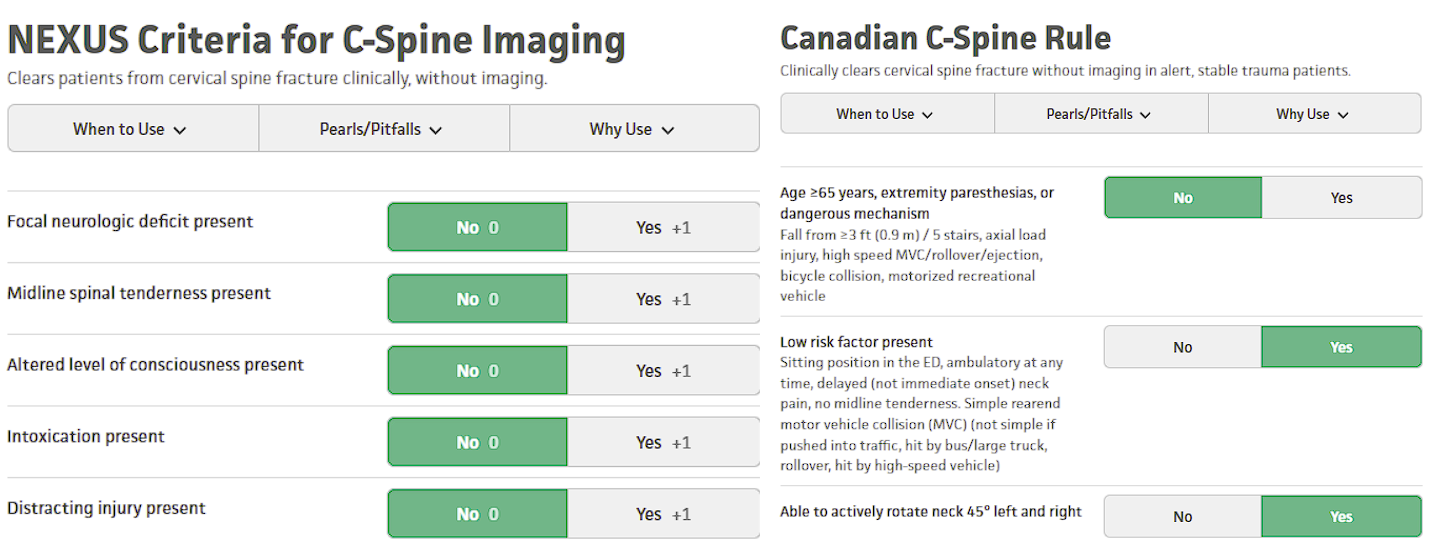
NEXUS Criteria (National Emergency X-Radiography Utilization Study)
A patient can be clinically cleared without imaging if all of the following are absent:
- Midline cervical tenderness
- Focal neurological deficit
- Altered level of consciousness (GCS < 15, intoxication)
- Intoxication (alcohol or drugs)
- Distracting injuries (e.g., fractures, significant pain elsewhere)
Canadian C-Spine Rule (CCR)
This rule is more specific than NEXUS and helps reduce unnecessary imaging. It follows a stepwise approach:
- High-risk features requiring imaging:
- Age ≥ 65 years
- Dangerous mechanism (e.g., fall from >3 feet, axial load, high-speed MVC. bicycle collision, Motor recreational vehicle)
- Paresthesias in extremities
- Low-risk features allowing clinical clearance if neck movement is adequate:
- Simple rear-end MVC
- Sitting position in ED
- Ambulatory at any time
- Delayed onset of neck pain
- No midline tenderness
- If the patient meets low-risk criteria and can actively rotate the neck ≥ 45° left and right, the C-collar can be removed without imaging.
Clinical Pearls & Pitfalls
Pearls:
- Use clinical decision rules to guide clearance and minimize unnecessary imaging.
- CT scan is the preferred imaging modality for patients requiring imaging due to its high sensitivity.
- Neurologic deficits warrant MRI, even if CT is normal, as ligamentous or spinal cord injuries may be present.
- Delayed presentations: Patients with persistent neck pain but a negative initial workup should receive outpatient follow-up and possibly MRI.
Pitfalls:
- Failure to recognize intoxication: Alcohol or drugs can mask pain, leading to premature clearance.
- Missing a distracting injury: Significant pain from another injury can prevent proper assessment.
- Relying on plain X-rays in high-risk cases: X-rays miss up to 30% of C-spine fractures; CT is preferred.
- Ignoring patient complaints: Even if the rules suggest clearance, persistent severe pain warrants further imaging. As a provider, use your best clinical judgement
Clinical Case 1
Case 1: A 45-year-old male presents after a MVC where he was rear ended by another vehicle at 10mph. He was wearing a seatbelt and denies any neck pain. He is alert (GCS 15), has no neurological deficits, no signs of intoxication.
Applying Clinical Decision Rules:
NEXUS Criteria:
- Midline tenderness: No
- Focal neurologic deficit: No
- Altered LOC: No
- Intoxication: No
- Distracting injury: No
✅ Meets all criteria — No imaging required.
Canadian C-Spine Rule:
- High-risk features: None
- Low-risk features: Ambulatory at scene, no midline tenderness
- Neck rotation: Able to rotate ≥ 45° bilaterally
✅ Meets criteria for clinical clearance.
Outcome: The patient demonstrates full active neck rotation. The C-collar is removed without imaging.
Clinical Case 2
Case 2: A 68-year-old male is brought in by EMS after falling from a ladder approximately 8 feet while cleaning gutters. He landed on his back and head. He is alert (GCS 15) but reports moderate neck pain. He denies numbness or weakness but appears uncomfortable when attempting to move his neck. There is midline cervical tenderness on exam.
Applying Clinical Decision Rules:
NEXUS Criteria:
- Midline tenderness: Yes
- Focal neurologic deficit: No
- Altered LOC: No
- Intoxication: No
- Distracting injury: No
❌ Fails NEXUS — Imaging required.
Canadian C-Spine Rule:
- High-risk factor present: Age ≥ 65 and dangerous mechanism (fall > 3 feet)
❌ Meets high-risk criteria — Imaging required.
Outcome: A non-contrast cervical spine CT is ordered, revealing a C6 vertebral body fracture. Neurosurgery is consulted, and the patient remains in a cervical collar with follow-up arranged.

C6 vertebral body fracture on CT
Discussion
Clearing the C-collar in the ED is a balance of patient safety and resource utilization. Overuse of imaging can lead to unnecessary radiation exposure and increased healthcare costs, while failure to identify a true C-spine injury can have devastating consequences. By applying validated decision rules like NEXUS and the Canadian C-Spine Rule, providers can make informed decisions that prioritize both safety and efficiency.
Clinical Case 3
Case 3: A 35-year-old female is brought in after a rollover motor vehicle collision at highway speeds. She was wearing a seatbelt and denies any loss of consciousness. She is alert (GCS 15), has no focal neurological deficits, and is not intoxicated. However, she reports moderate midline neck pain and has tenderness to palpation over the cervical spine.
Applying Clinical Decision Rules:
NEXUS Criteria:
- Midline tenderness: Yes
- Focal neurologic deficit: No
- Altered LOC: No
- Intoxication: No
- Distracting injury: No
❌ Fails NEXUS — Imaging required.
Canadian C-Spine Rule:
- High-risk features: Dangerous mechanism (high-speed rollover MVC)
❌ Meets high-risk criteria — Imaging required.
Outcome: A non-contrast cervical spine CT is performed and shows no acute fractures or dislocations. However, due to persistent midline tenderness, the patient is discharged home with a cervical collar in place and given instructions for neurosurgical or spine clinic follow-up. An outpatient MRI may be considered to evaluate for soft tissue or ligamentous injury if symptoms persist.
Outpatient Management & Considerations for MRI Follow-Up
For patients like the one in Clinical Case 3, where CT imaging shows no fractures but the patient still experiences persistent midline neck tenderness, it's important to continue monitoring and reassessing the patient’s condition after discharge.
1. Follow-Up Instructions:
The patient should be advised to follow up with a spine specialist or neurosurgeon within 1-2 weeks, or sooner if symptoms worsen.
Soft tissue or ligamentous injuries (such as sprains or strains) may not be visible on CT and can cause prolonged pain. MRI can help assess these soft tissues, especially if symptoms do not improve with conservative management.

MRI of the neck showing Ligamentum flavum tear from C7-T1 not seen on CT
Use of the cervical collar: Depending on the level of pain, the patient may be instructed to wear the collar for support for a short period. The use of a soft collar can help alleviate discomfort, though prolonged use should be avoided to prevent weakening of the neck muscles.
2. When to Consider MRI:
If symptoms such as neck pain, stiffness, or headaches persist beyond a few days despite conservative management, an MRI of the cervical spine is the next step in assessing for:
- Ligamentous injuries (e.g., sprains, tears)
- Spinal cord injury (e.g., contusions or edema that may not be visible on CT)
- Soft tissue swelling or damage
If the patient develops neurological symptoms such as weakness, tingling, or numbness in the extremities, MRI should be performed urgently to rule out any subtle spinal cord injury.
3. Red Flags for Immediate Reassessment:
- Worsening pain or new neurological deficits (e.g., numbness, tingling, weakness)
- Inability to tolerate neck movement or increasing pain with movement
- Signs of spinal cord compression such as bowel or bladder dysfunction, gait difficulties, or severe weakness
Conclusion:
Though CT imaging is invaluable for detecting fractures and dislocations, it has limitations in evaluating soft tissue injuries. For patients with midline tenderness and no visible fractures, MRI is an important tool for a more comprehensive assessment, especially if symptoms persist. Proper follow-up care is crucial to ensure that potentially significant soft tissue injuries are not missed and that the patient is managed appropriately.Key Takeaways:
- Use NEXUS or Canadian C-Spine Rule to guide clearance.
- If any high-risk feature is present, obtain imaging (CT preferred).
- If low-risk criteria are met and the patient has full active neck rotation, the collar can be removed without imaging.
- Remain cautious in patients with neurologic symptoms, intoxication, or distracting injuries.
By adhering to these principles, ED providers can ensure the safe and efficient clearance of C-spine collars, optimizing patient care and hospital resources.
Resources
- American College of Radiology. (n.d.). Appropriateness Criteria: Suspected Cervical Spine Trauma. Retrieved April 14, 2025. Learn More Here
- Eastern Association for the Surgery of Trauma. (n.d.). Cervical spine injury evaluation guidelines. Retrieved April 14, 2025. Learn More Here
- Grayline Medical. (n.d.). Aspen Medical Cervical Collars - Cervical Collar with Extra Pads (Adult Short). Retrieved April 14, 2025. Learn More Here
- Hoffman, J. R., Mower, W. R., Wolfson, A. B., Todd, K. H., & Zucker, M. I. (2000). Validity of a set of clinical criteria to rule out injury to the cervical spine in patients with blunt trauma. New England Journal of Medicine, 343(2), 94–99. Learn More Here
- MDCalc. (n.d.-a). Canadian C-Spine Rule. Retrieved April 14, 2025. Learn More Here
- MDCalc. (n.d.-b). NEXUS Criteria for C-Spine Imaging. Retrieved April 14, 2025. Learn More Here
- Radiopaedia.org. (n.d.). Post-traumatic ligamentum flavum tear. Retrieved April 14, 2025. Learn More Here
- Rosen, P., Barkin, R., Danzl, D., et al. (2018). Rosen’s Emergency Medicine: Concepts and Clinical Practice (9th ed.). Elsevier.
- Stiell, I. G., Wells, G. A., Vandemheen, K. L., Clement, C. M., Lesiuk, H., De Maio, V. J., ... & Reardon, M. (2001). The Canadian C-spine rule for radiography in alert and stable trauma patients. JAMA, 286(15), 1841–1848. Learn More Here
- Tintinalli, J. E., Stapczynski, J. S., Ma, O. J., et al. (2019). Tintinalli’s Emergency Medicine: A Comprehensive Study Guide (9th ed.). McGraw-Hill Education.



