Fluoroscopy for emergency department orthopedic reductions
Authors:
James Snitzer, MD; Alejandro Miranda, MD; Landon Mueller, MD
Case
A 12 yo boy soccer player presents by EMS from the local soccer tournament after he collided with another player. He fell to the ground with an outstretched hand to brace himself. EMS noted an obvious closed deformity to his wrist. X-rays reveal severely angulated and slightly displaced, distal radius and ulna fractures. His mother arrives, tearful, asking “will he need surgery?” As staff is preparing for the procedural sedation, there’s an extra tool that can set up for a successful reduction: fluoroscopy.

Mobile fluoroscopy, typically performed with a “C-arm” or “mini C-arm”, provides real-time x-ray imaging, producing live x-ray “video.” Clinicians can use fluoroscopy to guide joint and fracture reductions, with immediate visualization of reduction results. Fluoroscopy is not typically required for injuries such as a simple finger or shoulder dislocation that have adequate visual and tactile feedback. However, other injuries, most commonly radius, ulna, tibia and fibula fractures, are good candidates. Fractures located in the midshaft and those with a higher degree of displacement and angulation are more likely to be difficult reductions and may benefit from fluoroscopy.1,2 We believe there are several potential advantages of using fluoroscopy for joint and fracture reductions in the emergency department, including better reduction quality, success with maintaining the reduction, and time savings.3
Better reduction quality
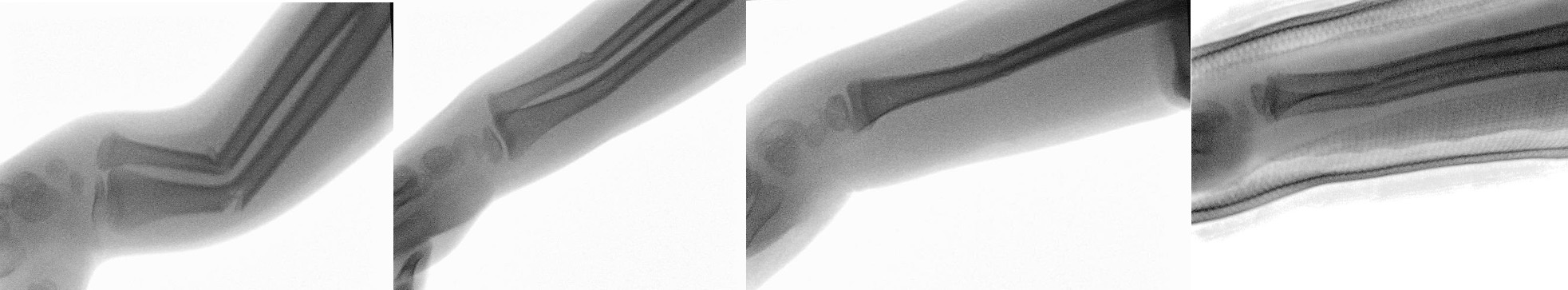
Fluoroscopy provides real-time visualization of a reduction, theoretically improving anatomical alignment. The evidence for this benefit is mixed, however, and it has not been well-studied in the emergency department. Two adult studies and one pediatric study comparing reductions with and without fluoroscopy guidance demonstrated no significant difference in reduction quality or need for surgery.4,5,6 Conversely, a retrospective cohort study of 279 wrist and forearm fractures found a significant improvement in reduction quality (measured by degrees of angulation) and need for surgery.3 Ultimately, these studies involved reductions performed by orthopedic surgeons, and there is potential that the visual cue from fluoroscopy could provide greater benefit to ED physicians who have less reduction experience. The images below provide an example of using fluoroscopy over the course of a reduction to improve anatomical alignment, including during splint application.
Success with maintaining the reduction
Maintaining anatomical position while splinting can be difficult for some fractures, particularly those with a high degree of joint instability. A classic example is an ankle fracture-dislocation. With the bony buttresses fractured in a trimalleolar ankle fracture, the talus easily disarticulates with the tibia. Fluoroscopy can help the clinician ensure adequate alignment and reduction while applying the splint and allowing it to set.

Time savings
Do the reduction correctly the first time, and it will be less likely to require revision. Having to re-sedate a patient to revise a previously placed splint is time-consuming and a pain for both the patient, yourself and your staff. The same study cited earlier demonstrated less need for re-reduction with use of fluoroscopy.3 It has also been shown to be adequate for post-reduction visualization, potentially removing the need for a traditional post-reduction radiograph. A review of 243 cases before and after an institutional policy change allowing fluoroscopy demonstrated no difference in need for re-reduction or surgery when relying on fluoroscopy. This and another study demonstrated an approximately 30 minute time savings in door to disposition when avoiding the post-reduction radiograph, even when considering the extra time to set up and use fluoroscopy during the sedation. However, if fluoroscopic images are not recorded in the medical record, formal post-reduction films should still be obtained.7,8,9
Radiation exposure
Fluoroscopy, when used in place of traditional radiography can also result in less radiation exposure to the patient. For context, a CT trauma pan-scan typically results in an exposure of around 34 mSV and OSHA cites 50mSV as the maximum annual occupational exposure.10,11 The previously mentioned pediatric study resulted in a mean 0.14 mSv for those undergoing fluoroscopy vs. 0.5 mSv for those with plain radiographs.3 Another retrospective review of operative orthopedic trauma patients demonstrated a mean exposure of 0.32 mSv for those undergoing operative fluoroscopy vs. 1.12 mSv for those managed with plain radiographs.10 Radiation exposure is greatest for the clinician and any assistants immediately close to the fluoroscopy machine. Moving several feet away significantly reduces the risk of radiation exposure. Once approximately 2 meters away from the machine, it becomes negligible and staff can further reduce the risk by utilizing lead shielding.12
Operating the c-arm
Like all other procedures, the best way to get good at using the c-arm, is to start using it. Familiarize yourself with your institutional policies on fluoroscopy in the ED. You may need to undergo credentialing and fluoroscopy training. When you have a reduction in the ED, remember to notify radiology early, and avoid having to wait for the c-arm to be brought to the patient’s room. Gown in led aprons appropriately and stand as far a distance as possible from the device to minimize radiation exposure.
Move the patient’s extremity as close to the detector side as possible. Obtain the best collimation possible, avoiding x-rays to areas away from the fracture site. Ensure that the c-arm is oriented perpendicular at 90 degrees to the extremity being imaged. Obtain both PA and lateral views of the fracture site. It’s important to obtain orthogonal views as a fracture can often be reduced in one plane but remain displaced in another.
Conclusion
After fluoroscopic-guided reduction under procedural sedation, the patient’s radius/ulna fracture was reduced to anatomical position with minimal angulation, and he was able to avoid surgery. When applied to the appropriate orthopedic injury, fluoroscopy can help achieve better reduction quality, maintain the reduction, and provide time savings in the ED.
References
- Rimbaldo KM, Fauteux-Lamarre E, Babl FE, Kollias C, Hopper SM. Deformed pediatric forearm fractures: Predictors of successful reduction by emergency providers. Am J Emerg Med. 2021;50:59-65.
- LaValva SM, Rogers BH, Arkader A, Shah AS. Risk factors for failed closed reduction of pediatric distal radius fractures. J Hand Surg Glob Online. 2020;2(4):196-202.
- Lee MC, Stone NE 3rd, Ritting AW, et al. Mini-C-arm fluoroscopy for emergency-department reduction of pediatric forearm fractures. J Bone Joint Surg Am. 2011;93(15):1442-1447.
- Menachem S, Sharfman ZT, Perets I, et al. Does fluoroscopy improve outcomes in paediatric forearm fracture reduction? Clin Radiol. 2016;71(6):616.e1-616.e5.
- Kazum E, Kadar A, Sharfman ZT, et al. Adult closed distal radius fracture reduction: Does fluoroscopy improve alignment and reduce indications for surgery? Hand (N Y). 2017;12(6):557-560.
- Dailey SK, Miller AR, Kakazu R, Wyrick JD, Stern PJ. The effectiveness of mini-C-arm fluoroscopy for the closed reduction of distal radius fractures in adults: A randomized controlled trial. J Hand Surg Am. 2018;43(10):927-931.
- Goodman AD, Walsh DF, Zonfrillo MR, Eberson CP, Cruz AI Jr. Fluoroscopy as definitive postreduction imaging of pediatric wrist and forearm fractures is safe and saves time. J Pediatr Orthop. 2020;40(1):e14-e18.
- Goodman AD, Zonfrillo MR, Chiou D, Eberson CP, Cruz AI Jr. The cost and utility of postreduction radiographs after closed reduction of pediatric wrist and forearm fractures. J Pediatr Orthop. 2019;39(1):e8-e11.
- Chitnis S, Giordano J, Naraghi L, Bonadio W. Utility of post-reduction radiographs after fluoroscopy-guided reduction and casting of uncomplicated pediatric forearm fractures. Pediatr Emerg Care. 2020;36(2):92-94.
- Wheeler JA, Weaver N, Balogh ZJ, et al. Radiation exposure in patients with isolated limb trauma: Acceptable or are we imaging too much? J Clin Med. 2020;9(11):3609.
- Occupational Safety & Health Administration. Radiation emergency preparedness and response. U.S. Department of Labor. Learn More
- Thibault J, Naciri W, Rouleau DM, Chapleau J. Intraoperative radiation exposure in a level 1 trauma centre orthopedic operating room. Can J Surg. 2025;68(3):E235-E241.
ACEP Now Newsletter Article Submission
References Summary
-- Pediatrics --
Lee MC, Stone NE 3rd, Ritting AW, Silverstein EA, Pierz KA, Johnson DA, Naujoks R, Smith BG, Thomson JD. Mini-C-arm fluoroscopy for emergency-department reduction of pediatric forearm fractures. J Bone Joint Surg Am. 2011 Aug 3;93(15):1442-7.
Improvement in reduction quality (measured by avg. angulation), decreased need for fracture reduction, need for surgery, overall radiation exposure, total orthopedics consultation time - all were significant
Goodman AD, Walsh DF, Zonfrillo MR, Eberson CP, Cruz AI Jr. Fluoroscopy as Definitive Postreduction Imaging of Pediatric Wrist and Forearm Fractures Is Safe and Saves Time. J Pediatr Orthop. 2020 Jan;40(1):e14-e18.
Sedation times were longer under fluoroscopy but did not increase total ED time
Fluoroscopy as definitive imaging was associated with 33 min shorter ED stay and did not increase need for re-manipulation or surgery
Goodman AD, Zonfrillo MR, Chiou D, Eberson CP, Cruz AI Jr. The Cost and Utility of Postreduction Radiographs After Closed Reduction of Pediatric Wrist and Forearm Fractures. J Pediatr Orthop. 2019 Jan;39(1):e8-e11.
Post-reduction radiographs did not change management. Associated with 26.2 min longer stay and 2.6% of the encounter cost
Menachem S, Sharfman ZT, Perets I, Arami A, Eyal G, Drexler M, Chechik O. Does fluoroscopy improve outcomes in paediatric forearm fracture reduction? Clin Radiol. 2016 Jun;71(6):616.e1-5.
No difference in re-reduction and surgery rates
Chitnis S, Giordano J, Naraghi L, Bonadio W. Utility of Post-reduction Radiographs After Fluoroscopy-Guided Reduction and Casting of Uncomplicated Pediatric Forearm Fractures. Pediatr Emerg Care. 2020 Feb;36(2):92-94.
Post-reduction radiographs after fluoroscopy have “little clinical utility and contributes to increased radiation exposure, patient health care cost, and time spent in the ED.” *Midshaft radius-ulna displaced/angulated could be beneficial
-- Adults --
Kazum E, Kadar A, Sharfman ZT, Otremsky H, Gigi R, Rosenblatt Y, Dolkart O, Pritsch T. Adult Closed Distal Radius Fracture Reduction: Does Fluoroscopy Improve Alignment and Reduce Indications for Surgery? Hand (N Y). 2017 Nov;12(6):557-560.
No significant difference in need for surgery or post-reduction alignment with fluoroscopy
Dailey SK, Miller AR, Kakazu R, Wyrick JD, Stern PJ. The Effectiveness of Mini-C-Arm Fluoroscopy for the Closed Reduction of Distal Radius Fractures in Adults: A Randomized Controlled Trial. J Hand Surg Am. 2018 Oct;43(10):927-931.
Equivalent post-reduction parameters and rate of initial operative management
Rimbaldo KM, Fauteux-Lamarre E, Babl FE, Kollias C, Hopper SM. Deformed pediatric forearm fractures: Predictors of successful reduction by emergency providers. Am J Emerg Med. 2021 Dec;50:59-65.
Midshaft location and higher degree of angulation are more likely to be difficult reductions
LaValva SM, Rogers BH, Arkader A, Shah AS. Risk Factors for Failed Closed Reduction of Pediatric Distal Radius Fractures. J Hand Surg Glob Online. 2020 Jun 9;2(4):196-202.
Higher degree of angulation, cast index>0.8 are more likely to be unsuccessful.
Cast index <0.8 is desired (saggital width/coronal)
Wheeler JA, Weaver N, Balogh ZJ, Drobetz H, Kovendy A, Enninghorst N. Radiation Exposure in Patients with Isolated Limb Trauma: Acceptable or Are We Imaging Too Much? J Clin Med. 2020 Nov 9;9(11):3609. doi: 10.3390/jcm9113609.
Occupational Safety & Health Admin., Radiation Emergency Preparedness and Response, U.S. Dep’t of Labor
Thibault J, Naciri W, Rouleau DM, Chapleau J. Intraoperative radiation exposure in a level 1 trauma centre orthopedic operating room. Can J Surg. 2025 Jun 10;68(3):E235-E241. doi: 10.1503/cjs.003824.