Stayin Alive! Stayin Alive! A Clinical Case Demonstrating the Utility of the Mid-Esophageal Long Axis View in Resuscitative TEE
Chelsea Bunce, DO
Jordan Tozer, MD
Virginia Commonwealth University
Case Presentation
A 64-year-old male presented to the Emergency Department after being found unresponsive at home. Family members reported that the patient experienced sudden chest pain, followed by collapse and loss of consciousness. Upon arrival to the ED, the patient was in cardiac arrest with pulseless electrical activity (PEA) on the ECG. CPR was immediately initiated by the ED team, and the patient was intubated. Resuscitation proceeded with multiple rounds of epinephrine given and ongoing CPR, but the team was concerned that despite high-quality chest compressions, the patient’s condition was not improving and return of spontaneous circulation (ROSC) had not been achieved.
Background
Obtaining the view
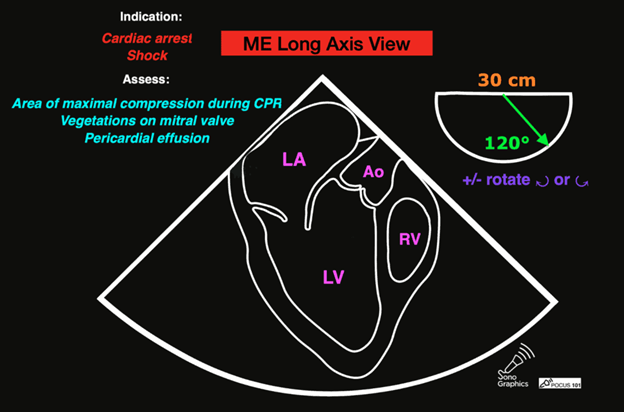
The TEE mid-esophageal long axis view (ME-LAX) is the mirror image of the parasternal long axis view in transthoracic echo (TTE), with the left atrium closest to the probe face and the right ventricle (RV) furthest from the probe. To achieve this view, the TEE probe is inserted approximately 30-35cm until a mid-esophageal four chamber view is obtained. From this starting point, the omniplane is rotated to 120 degrees, then further fine adjustments are made to the omniplane and probe rotation until a view showing both mitral inflow and aortic outflow to the left ventricle (LV) is achieved (Fig. 1). This view is excellent for evaluating LV contractility and assessing aortic and mitral valve function.1 During resuscitation, this view is key to real-time evaluation of CPR effectiveness.
 Figure 1. TEE ME-LAX view showing severely reduced ejection fraction (EF) following ROSC
Figure 1. TEE ME-LAX view showing severely reduced ejection fraction (EF) following ROSC
Overview of findings
The mid-esophageal long-axis view provides comprehensive insight into the heart's function including the left ventricle's size and contractility, mitral valve performance, and the presence of pericardial effusion. This view also enables the assessment of the aortic root and arch, the interventricular septum, and right ventricle. Finally, it provides a great view to assess the effectiveness of CPR.2
Specifics
The ME-LAX view provides one of the best views for evaluating the mitral valve. It allows for the assessment of mitral valve motion, leaflet integrity, and presence of regurgitation. It is useful for evaluating mitral valve prolapse or mitral regurgitation.2
This view offers excellent assessment of the aortic valve, aortic root, and ascending aorta. It can be used to identify aortic pathologies such as aortic stenosis, aortic regurgitation or dilation of aortic root.2
The ME-LAX view is important for evaluating left ventricular size and function when assessing for heart failure or ischemic disease.2 The view helps assess the dimensions of left ventricle, evaluation of wall motion abnormalities, estimation of ejection fraction, and is important for evaluating the ventricular contractility.1
Most importantly for the resuscitationist, the ME-LAX view is used to evaluate the quality of CPR and hand placement for chest compressions; so it should be obtained during initiation of CPR and even when changing CPR providers if possible. Optimal chest compressions should result in vigorous LV squeeze with near concurrent aortic valve opening (Figure 2). Incorrect compressions, usually too high on the chest wall, will result in LV outflow obstruction and ineffective CPR (Figure 3). This can be seen on the ME-LAX view as squeeze over the AV itself, narrowing of the aortic outflow tract, absence of LV compression and/or absence of aortic valve opening during compressions. Signs of ineffective CPR should prompt adjustments in compression location and/or depth and subsequent re-evaluation for effectiveness.2
 Figure 2. Me-LAX view during CPR (slowed to 50% speed) showing mid-LV compression with concurrent aortic valve opening
Figure 2. Me-LAX view during CPR (slowed to 50% speed) showing mid-LV compression with concurrent aortic valve opening
 Figure 3: ME-LAX view during CPR (slowed to 50% speed) showing complete compression of the aortic root during CPR
Figure 3: ME-LAX view during CPR (slowed to 50% speed) showing complete compression of the aortic root during CPR
Case Resolution
The team performs the ME-LAX view to assess the left ventricle, mitral valve and left ventricular outflow tract in real time. The image shows that the LVOT is not opening well due to improper hand placement during compressions. The team recommended moving the compressors’ hands slightly lower on the sternum and near the xiphoid process to increase the force applied to the left ventricle and reduce the force on the LVOT. After the repositioning, the LV was noted to be squeezing more vigorously with concurrent AV opening with each compression. This adjustment improved the cardiac output and after a few more rounds of adjusted CPR and continued ACLS, ROSC was achieved
Summary
The mid-esophageal long-axis view is an important echocardiographic perspective during CPR as it provides real-time visualization of the heart's anatomy and function.2 This view helps guide CPR interventions by allowing clinicians to assess cardiac motion, ventricular filling, and the effectiveness of chest compressions. It also aids in identifying the underlying cause of the arrest, such as pericardial effusion or cardiac tamponade. In situations like advanced cardiac life support (ACLS), the mid-esophageal long axis view can enhance decision-making, optimize the timing of interventions, and improve patient outcomes by ensuring targeted, efficient resuscitation efforts.1
Resources
- Guidelines for the Use of Transesophageal Echocardiography (TEE) in the ED for Cardiac Arrest. Ann Emerg Med. 2017;70(3):442-445. doi:10.1016/j.annemergmed.2017.06.033.
- Hahn RT, Abraham T, Adams MS, et al. Guidelines for Performing a Comprehensive Transesophageal Echocardiographic Examination: Recommendations from the American Society of Echocardiography and the Society of Cardiovascular Anesthesiologists. J Am Soc Echocardiogr. 2013;26(9):921-964. doi:10.1016/j.echo.2013.07.009