Ultrasound Guided Advanced Cardiovascular Life Support
- Rachel B. Liu, MD, FACEP
- Felipe Aguayo-Romero, MD, FACEP
Introduction
Advanced Cardiovascular Life Support (ACLS) guidelines published by the American Heart Association provide algorithms that assist in the identification and management of suspected stroke, acute coronary syndrome, and cardiac arrhythmias including asystole, pulseless electrical activity (PEA), bradycardia, tachycardia, pulseless ventricular tachycardia, and ventricular fibrillation.
- Bedside ultrasound may be used as a diagnostic and prognostic aid for patients in cardiac arrest and is recommended as an adjunct to patient evaluation in the hands of qualified operators.1
Current Limitations in ACLS
Across multiple studies, the accuracy of manual pulse checks is poor.2-4
Identifying intervenable arrhythmias may be difficult in the absence of a strong pulse or without dedicated EKG tracings.
- Eg, identifying the root cause for true PEA vs. “pseudo PEA”
- Eg, identifying fine ventricular fibrillation which may not appear on the monitor or EKG tracings.
Identifying the etiology of cardiac arrest may be difficult without the ability to obtain a description of events or past medical history.
These are areas which may be aided by performing ultrasound during cardiac arrest.
Pulse Identification
Primarily, the carotid or femoral artery is identified in the vessel’s short axis using a linear transducer.
Site selection should be determined by provider preference, team size, and environment in each specific scenario.
- For small teams where the ultrasonographer may be at the head of the bed, the carotid artery may be a reasonable target.
- The carotid artery is identified by placing the transducer in a transverse orientation on the anterolateral portion of the neck just over the sternocleidomastoid muscle. It is most commonly located medial to the internal jugular vein. However, anatomical variants are not uncommon.5
- For large teams in which access to the head of the bed is more limited, the femoral artery may be the more suitable site.
- The femoral artery is identified by placing the linear transducer such that it is aligned with the inguinal ligament (located between anterior inferior iliac spine and pubic tubercle). The femoral artery will be located lateral to the femoral vein.
B-Mode Pulsatility: Once either vessel is identified, pulsatility may be assessed visually by carefully looking for rhythmic expansile distortion in the arterial walls or surrounding tissues.
- The presence of pulsatility during the rhythm check pause indicates that ROSC has been achieved. However, interpretation may be subjective and operator-dependent.
Doppler Pulsatility using Pulse Wave Doppler:6
- Whenever possible, the sonographer should begin imaging the artery and selecting the pulse wave Doppler function during the final 10 seconds of a chest compression cycle.
- This technique will allow capture of pulsation Doppler tracings during ongoing CPR.
- During the rhythm check pause, absence of continued spontaneous tracings indicates that ROSC has not been achieved.
- A continuation of spontaneous pulse wave tracings during the rhythm check indicates ROSC.
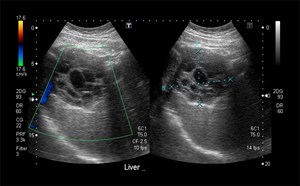
Case 1, Video 1.
A patient weighing over 400 lbs arrested in the ED. Physical examination and echocardiography were not achievable. This video shows the internal jugular vein (vessel superficial) and carotid artery (vessel deeper) during compressions. Video courtesy of Yale School of Medicine, Emergency Department.
Case 1, Image 1.
Pulse wave Doppler started during ongoing compressions (with high amplitude tracings that alias). Image courtesy of Yale School of Medicine, Emergency Department.
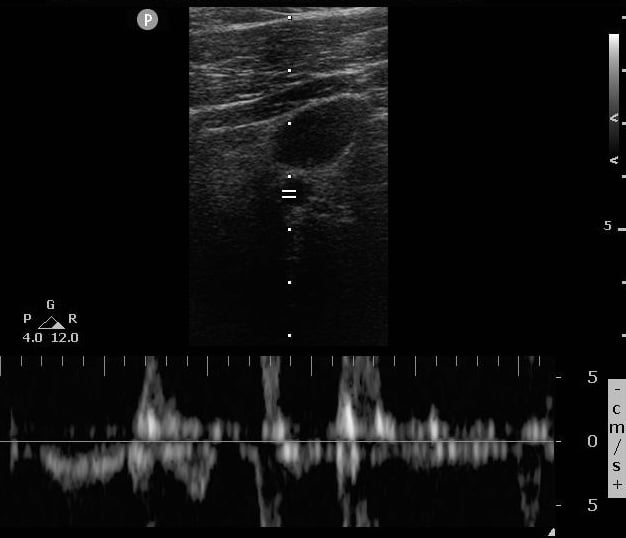
Case 1, Image 2.
Sustained regular Doppler pulsations during the pause, indicated ROSC. Image courtesy of Yale School of Medicine, Emergency Department.
Transthoracic Echocardiography (TTE) During CPR
Directly visualizing cardiac physiology during ACLS may allow rapid identification of the underlying cause for the arrest and immediate management. This may include cardiac tamponade, right ventricular strain in the setting of pulmonary embolism, cardiogenic or hypovolemic shock.
Of note, performance of TTE during the pulse check pause has been shown to create significant prolongation of the pause, undermining efforts to promote forward circulation.7-8
However, the following are strategies to perform TTE during CPR and retain a pause duration of less than 10 seconds:9
- The most experienced sonographer should acquire the images
- The sonographer should find the most optimal view of the heart before the CPR pause.
- The sonographer should initially focus on acquiring images with the best possible quality, as interpretation may be reviewed when CPR resumes.
- If manual compressions are being performed, towels should be readily available or placed over the sonographer’s hand to rapidly wipe gel from the chest wall.
- The sonographer should relay important findings to the team regarding reversible causes for the arrest or visualization of an organized myocardial activity/arrhythmia
Visualization of the left ventricle during compressions may also allow evaluation of compression adequacy regarding the frequency and timing, vector of force, pressure and location of compressions.10
- Compressions are adequate if full LV compression with subsequent luminal expansion during chest wall recoil is seen.
- Compressions are inadequate if the above is not seen, or the vector of force is not visualized over the left ventricle.
Case 2, Video 1.
A mechanical compression device was used to provide compressions. In this parasternal long axis view, notice how the movement and vector of force is all on the patient’s right side, over the right ventricle, ascending aorta and left atrium. There is no force applied to the left ventricle. Video courtesy of Yale School of Medicine, Emergency Department.
Case 2, Video 2.
Compressions were switched to manual delivery, and evaluated using a subxiphoid view, with compression force moved more towards the patient’s left side. Note that the LV has full compression and then luminal expansion during recoil. Video courtesy of Yale School of Medicine, Emergency Department.
Performing TTE during chest compressions or during the pause in the compression cycle is not an easy task and imaging cannot be achieved in all patients. This is the reason that emergency departments are pursuing efforts towards transesophageal echo (TEE, see below section).
Identifying Cardiac Arrest Etiology and Arrhythmias
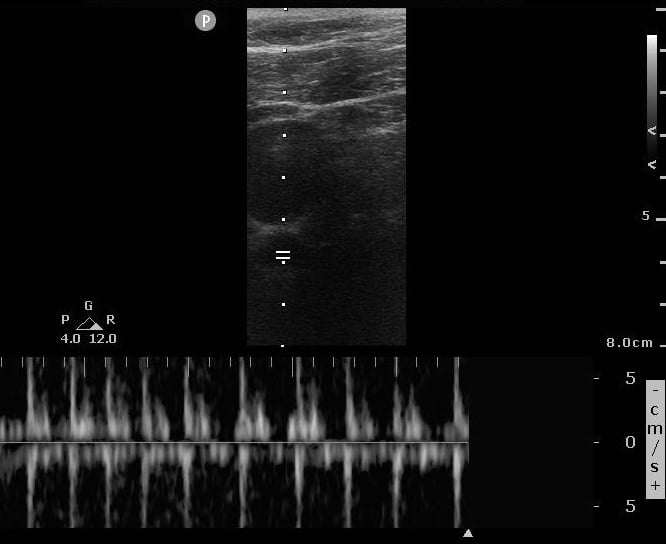
POCUS aids identification of reversible causes for arrhythmias and arrest, known as the H’s and T’s of ACLS. (Figure 1) POCUS may also identify other causes not listed.
- See the Cardiac chapter for more information about assessing for pericardial effusion and tamponade, as well as right ventricular strain (pulmonary embolus).
- This allows for immediate treatments that may not be part of the ACLS algorithms.
Figure 1.
H’s and T’s with highlighted areas that may be identified by POCUS
Case 3, Video 1.
Subxiphoid view of a cardiac arrest patient with no motion (standstill) but a large right ventricle with clotting blood and septal bowing, indicative of right heart strain presumably from a large pulmonary embolus. Video courtesy of Yale School of Medicine, Emergency Department.
Case 3, Video 2.
TPA was pushed and ongoing ACLS resulted in meaningful, organized cardiac activity by the next pause in compressions. Video courtesy of Yale School of Medicine, Emergency Department.
Case 3, Video 3.
10 minutes after TPA was administered, the patient fully regained ROSC. Video courtesy of Yale School of Medicine, Emergency Department.
Intra-arrest echocardiography also allows assessment for shockable rhythms that may not appear on the monitor or EKG rhythm strips, such as fine ventricular fibrillation.
This leads to defibrillation as an option, while without visualization on ultrasound, the rhythm would likely have been deemed as PEA and non-shockable.
Case 4, Video 1.
Subxiphoid view of a cardiac arrest patient (note atypical appearance) in which the etiology of the arrest (tamponade), and adequacy of compressions are visible in the same view. Video courtesy of Yale School of Medicine, Emergency Department.
Case 4, Video 2.
During the pause, both the tamponade and myocardial and valvular fibrillation (ventricular fibrillation) can be seen. This patient subsequently had an emergent pericardiocentesis and defibrillation. Video courtesy of Yale School of Medicine, Emergency Department.
Case 4, Video 3.
This parasternal long axis view shows ROSC, with the ascending aorta dilated over 4 cm, indicating a likely aortic dissection that is causing the tamponade and arrest. A significant pericardial effusion is still seen post-pericardiocentesis. Video courtesy of Yale School of Medicine, Emergency Department.
Resuscitative Transesophageal Echocardiography (TEE)
TEE is becoming increasingly available in emergency departments. While additional technical skill is required, it provides significant advantages over transthoracic echocardiography:
- Acoustic windows are independent from body habitus and image quality is consistently excellent. This makes TEE an optimal tool for guiding CPR.
- Once placed, imaging is continuous and there is no delay in the CPR pause for image acquisition. TEE is associated with shorter pauses than TTE.11
- As an internal device, it will not hinder devices that need to be placed on the chest wall (eg, defibrillator pads, mechanical compression devices), nor will it be disrupted by those devices.
TEE Probe Anatomy:
- Transducer tip - the piezoelectric crystals are located here. The plane of the sound beam can be rotated from 0° (neutral) to 180° (mirror image).
- Shaft - contains the wiring and has depth markers to measure from lip level
- Hanging ring – often present on handle and can be used to hang the probe from a pole, freeing the operator’s hand while providing continuous image.
- Bite block - not part of the equipment, but a necessary component to prevent damage to the probe
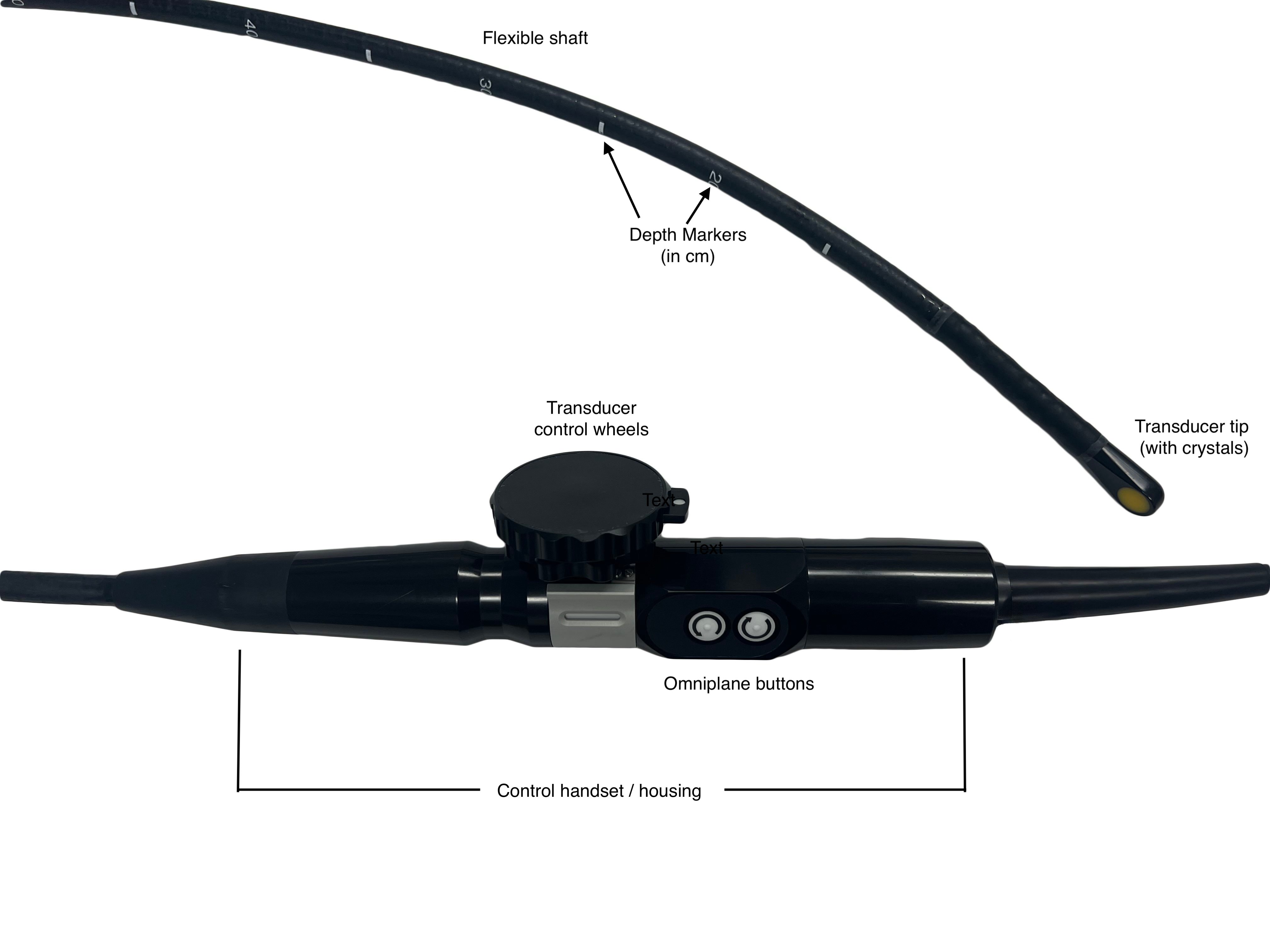
Figure 2.
The labeled parts of a transesophageal transducer
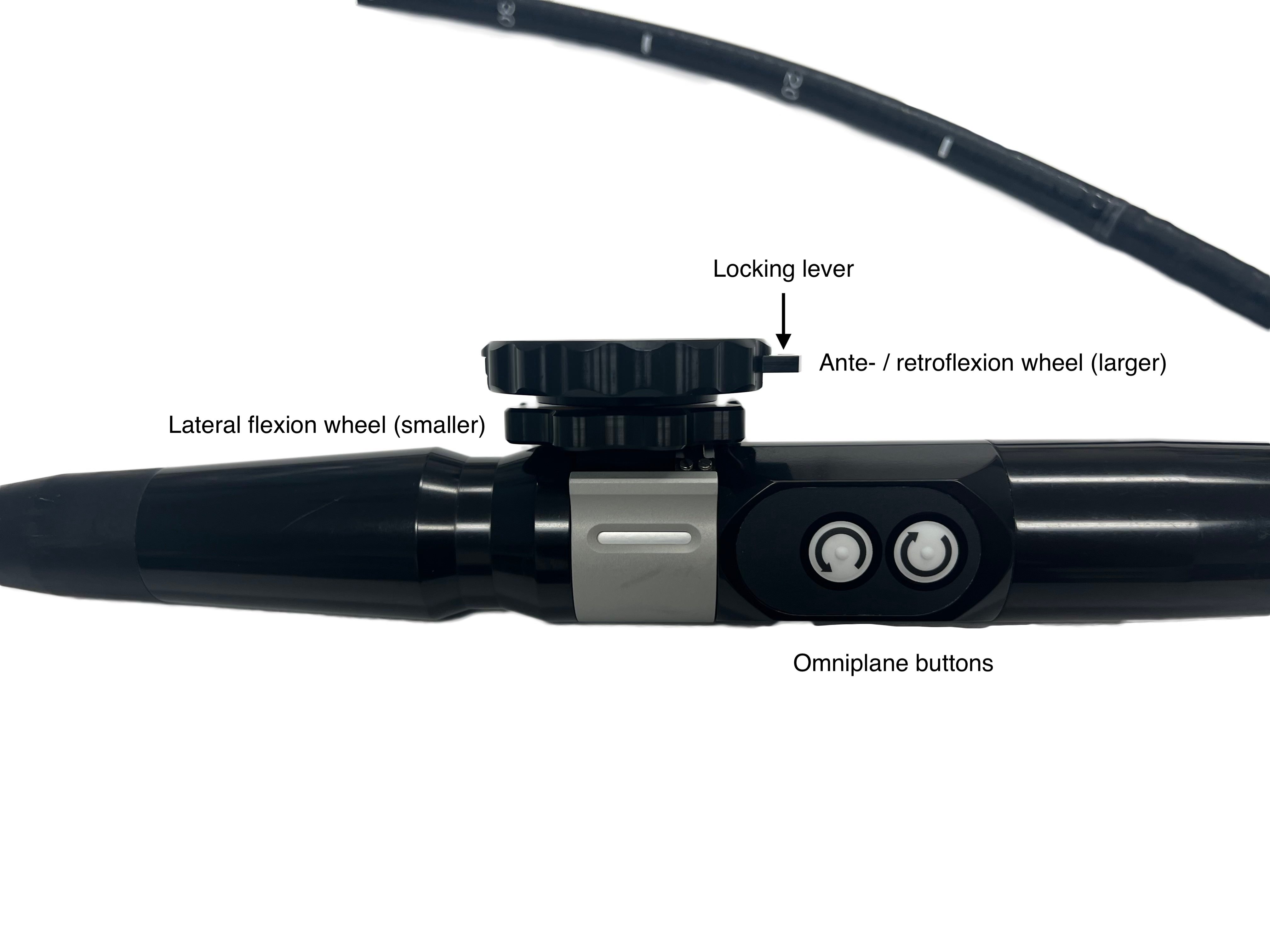
Figure 3.
The TEE controls
Controls
- Anteflexion/Retroflexion wheel (large wheel) - flexes the probe head anteriorly or posteriorly
- Lateral flexion wheel (small wheel) - flexes the probe head left or right. This control is used infrequently in resuscitative TEE.
- Omniplane buttons - this rotates the piezoelectric crystals’ plane to provide a wide variety of views
- Locking lever - will lock probe in current position. Avoid activating it as advancing or withdrawing the probe in a locked position may cause trauma to the esophagus or stomach.
Basic Views in Resuscitative TEE:12
Midesophageal 4 chamber view
- Often the easiest view to obtain
- Advance the probe to approximately 35 cm from the lip and apply slight retroflexion to avoid ventricular foreshortening.
- View is analogous to the transthoracic apical 4 chamber view allowing all chambers to be viewed simultaneously
- Tip: Slight withdrawal of the probe will provide a midesophageal 5 chamber view, providing visualization of the left ventricular outflow tract
Midesophageal long axis view
- At the same 35 cm depth, rotate the multiplane to 130-140°.
- View is analogous to the transthoracic parasternal long axis view allowing visualization of the left ventricle, left atrium, left ventricular outflow tract, and proximal aorta.
Midesophageal bicaval view
- At the same 35 cm depth, rotate the multiplane to 90° and rotate the probe to the patient’s right until the left atrium, right atrium, superior vena cava, and inferior vena cava are imaged simultaneously.
- he superior vena cava will be located at the same side of the screen as your indicator.
Transgastric short axis view
- With the multiplane returned to 0°, advance the probe into the stomach and apply anteflexion.
- View is analogous to the transthoracic parasternal short axis view showing the left ventricular cavity with the papillary muscles and the right ventricle.
Guiding ACLS with TEE
- Similar to transthoracic echocardiography, reversible cause for cardiac arrest and true arrhythmias may be assessed with better image quality than TTE.
- The high quality imaging provided also allow it to guide the performance of CPR regarding compression location and adequacy.
- Views typically used are the midesophageal 5 chamber, or the midesophageal long axis view.
- Both views provided imaging of the left ventricle, the left ventricular outflow tract, the aortic valve and the aortic root.
- Adequate CPR should correlate with opening of the aortic valve during compressions.
- If the area of maximal compression occurs over the ascending aorta, aortic outflow tract, or left ventricular outflow tract instead of the body of the left ventricle, forward flow may be impeded. However, CPR is often performed at the distal third of the sternum, which may place maximal compression directly over those areas.10,12-14
Case 5, Video 1.
In this cardiac arrest patient, a transthoracic echo was performed first, without good image quality achieved. Video Courtesy of Vi Dinh (POCUS 101).
Case 5, Video 2.
A TEE was performed with much better visualization, so much so that organized cardiac activity was seen and then manual compressions were started. Note the full compression of the left ventricle and subsequent expansion during recoil. Video Courtesy of Vi Dinh (POCUS 101).
Case 6, Video 1.
Example of right-sided, not left, ventricular compressions during CPR in a transgastric short axis view. Video Courtesy of the Hospital of the University of Pennsylvania (Penn Medicine), Department of Emergency Medicine.
Case 6, Video 2.
Example of right-sided, not left, ventricular compressions during CPR in a midesophageal 5 chamber view. Video Courtesy of the Hospital of the University of Pennsylvania (Penn Medicine), Department of Emergency Medicine.
References
- Link MS, Berkow LC, Kudenchuk PJ, et al. Part 7: Adult advance cardiovascular life support: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132(18): S444-S464.
- Westafer L. Stop performing routine pulse checks during CPR. ACEP Now. 2022 August 2;41(8):1-2. Learn More
- Tibballs J, Weeranatna C. The influence of time on the accuracy of healthcare personnel to diagnose paediatric cardiac arrest by pulse palpation. Resuscitation. 2010;81(6):671-5.
- Eberle B, Dick WF, Schneider T, Wisser G, Doetsch S, Tzanova I. Checking the carotid pulse check: diagnostic accuracy of first responders in patients with and without a pulse. Resuscitation. 1996;33(2):107-116.
- Lim CL, Keshava SN, Lea M. Anatomical variations of the internal jugular veins and their relationship to the carotid arteries: a CT evaluation. Australas Radiol. 2006;50(4):314-8. (doi:10.1111/j.1440-1673.2006.01589.x)
- Cohen AL, Li T, Becker LB, et al. Femoral artery Doppler ultrasound is more accurate than manual palpation for pulse detection in cardiac arrest. Resuscitation. 2022;173:156-65.
- Clattenburg EJ, Wroe P, Brown S, et al. Point-of-care ultrasound use in patients with cardiac arrest is associated prolonged cardiopulmonary resuscitation pauses: A prospective cohort study. Resuscitation. 2018;122:65-8.
- Huis In 't Veld MA, Allison MG, Bostick DS, et al. Ultrasound use during cardiopulmonary resuscitation is associated with delays in chest compressions. Resuscitation. 2017;119:95-8.
- Clattenburg EJ, Wroe PC, Gardner K, et al. Implementation of the Cardiac Arrest Sonographic Assessment (CASA) protocol for patients with cardiac arrest is associated with shorter CPR pulse checks. Resuscitation. 2018;131:69-73.
- Liu RB, Bogucki S, Marcolini EG, et al. Guiding Cardiopulmonary Resuscitation with Focused Echocardiography: A Report of Five Cases. Prehosp Emerg Care. 2020;24(2):297-302.
- Fair J, Mallin MP, Adler A, et al. Transesophageal echocardiography during cardiopulmonary resuscitation is associated with shorter compression pauses compared with transthoracic echocardiography. Ann Emerg Med. 2019;73(6):610-6.
- Teran F, Dean AJ, Centeno C, et al. Evaluation of out-of-hospital cardiac arrest using transesophageal echocardiography in the emergency department. Resuscitation. 2019;137:140-7.
- Catena E, Ottolina D, Fossali T, et al. Association between left ventricular outflow tract opening and successful resuscitation after cardiac arrest. Resuscitation. 2019;138:8-14.
- Chu SE, Huang CY, Cheng CY, et al. Cardiopulmonary resuscitation without aortic valve compression increases the chances of return of spontaneous circulation in out-of-hospital cardiac arrest: a prospective observational cohort study. Crit Care Med. 2024;52(9):1367-79.