Musculoskeletal Ultrasound – Overview
John P. Gullett, MD and Jonathan F. Swanson, MD, DTMH, FACEP
1. Introduction and Indications
Point-of-care ultrasonography (POCUS) offers the emergency physician (EP) numerous applications for diagnosing musculoskeletal pathology and guiding procedures. Many of these applications are straightforward and require minimal training while providing valuable emergent clinical information.1-17
Musculoskeletal POCUS may be superior to conventional radiographs in some cases, such as fractures of the ribs and sternum.14-16
Its use is increasingly appreciated in resource-limited, disaster, and military settings.17
Indications include investigating fractures, effusions, bursitis, dislocations, and tendon injuries, as well as procedural guidance for hematoma blocks of fractures, fracture reduction, peripheral nerve blocks, foreign body removal, and arthrocentesis.
2. Anatomy
Bones
Bright hyperechoic lines with no echoes deep to the densely calcified cortex. Ultrasound can only view the surface of bones.
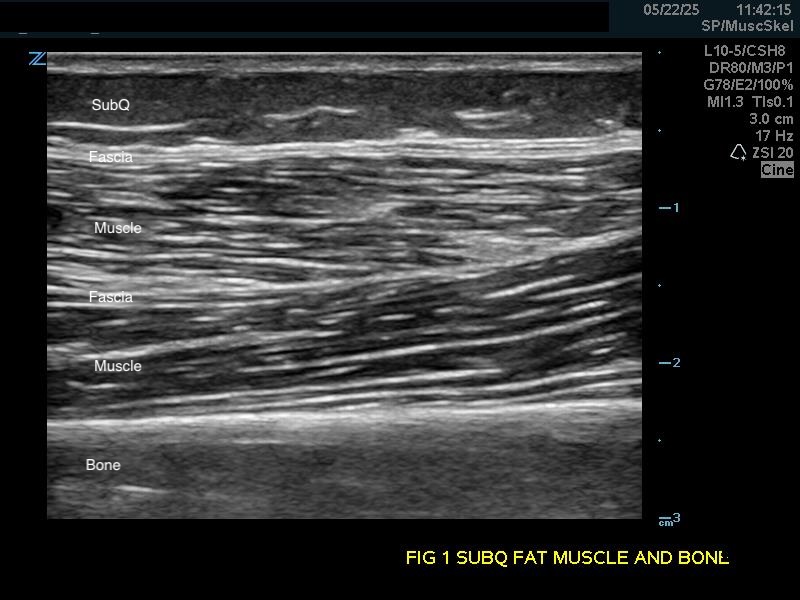
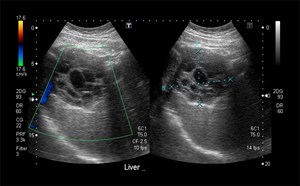
Figure 1a.
(A) Longitudinal view. Bone appears as a distinct bright echogenic line with no visible structures beneath, Subcutaneous fat appears relatively hypoechoic with thin septations of connective tissue.
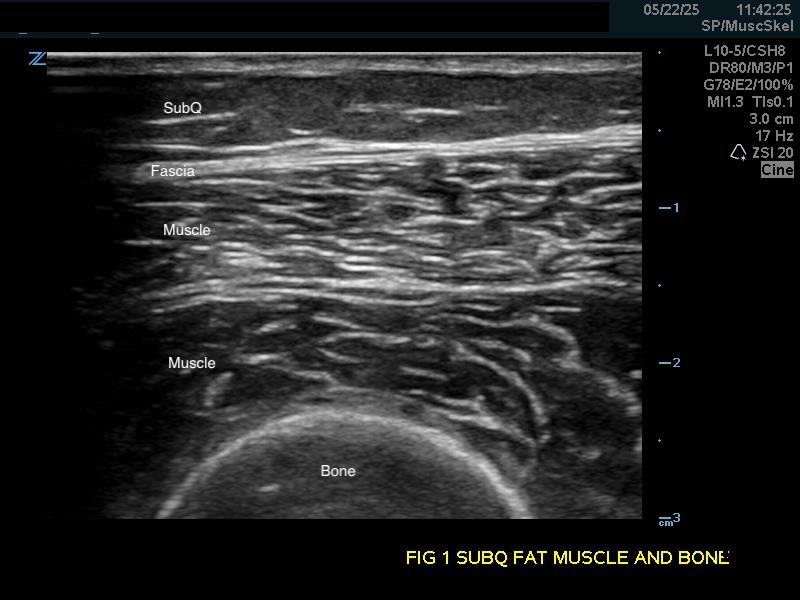
Figure 1b.
Transverse view.
Soft Tissue
Subcutaneous fat: Relatively hypoechoic with thin septations of connective tissue. The thickness of this layer varies and may require increasing the depth setting of your machine.
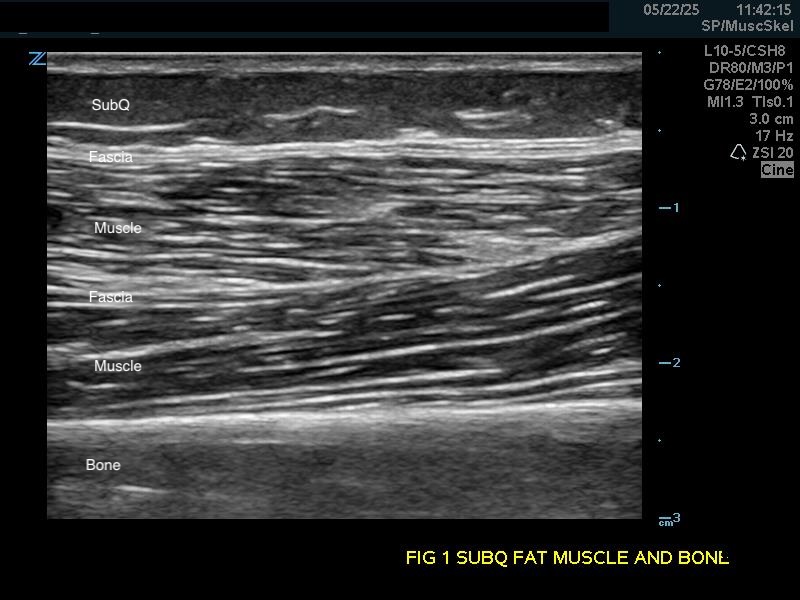
Figure 1a.
Longitudinal view. Bone appears as a distinct bright echogenic line with no visible structures beneath, Subcutaneous fat appears relatively hypoechoic with thin septations of connective tissue.
Muscle: Longitudinally, appears as slabs of striated hypoechoic tissue contained within the thin hyperechoic lines of fascia. Viewed transversely, muscle striations or septa appear dotted and punctate or form short lines. Fascial lines separate muscle compartments.
Video 1a.
Longitudinal view of muscle and, fascia using a linear transducer.
Tendons and Ligaments: Longitudinally, tendons have a narrow, densely striped fibrillar appearance of parallel lines. They are more echogenic and more densely striated than muscle. Transversely, appear as round or flattened ovals with a punctate interior. Tendons cause anisotropy, an artifact that shows dark areas within the tendon, which can be mistaken for tears or defects (see below). Ligaments appear similar to tendons but tend to be more irregular and difficult to discern, with the exception of the patellar ligament, which appears similar to its proximal quadriceps tendon.4
Video 2a.
(A) Quadriceps tendon where it inserts into the superior patellar bone (B) Distal patellar ligament, that has the same echotexture as tendons, originating from the inferior patella to the proximal tibial tuberosity.
Video 2c.
Short axis of the Achilles tendon with the transducer sliding distally to the calcaneus.
Synovial Bursa: Not often visualized (potential space). May normally contain 4 mL of fluid or more if inflamed or infected.
Hyaline Articular Cartilage: Appears as a thin very hypoechoic rim over a hyperechoic bony cortex. It is so hypoechoic it may be confused with fluid.
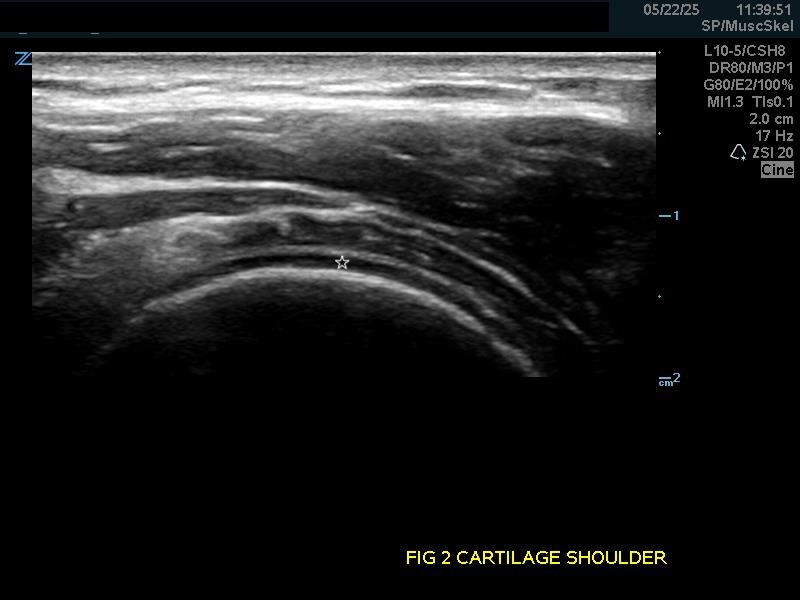
Figure 2.
(A) Hyaline articular cartilage (star) of the shoulder and (B) knee.
Nerves: Seen running along fascial planes, often paired with blood vessels, and within muscles themselves. Longitudinally, they appear as hyperechoic fibrinous cords, similar to tendons but more hyperechoic. Viewed transversely, the nerve fascicles give a "honeycomb" appearance and are less densely fibrillar than tendons.
Video 1b.
Short axis tracing of the forearm showing the median nerve with the transducer sliding proximally up the forearm.
3. Scanning Technique and Normal Findings
Use a high-frequency linear array transducer (7-12 MHz), which offers higher resolution images of superficial structures. Other transducers may be needed for larger or deeper structures.

Figure 3.
High-frequency linear array transducer (7-12 MHz), which offers higher resolution images of superficial structures and recommended for most musculoskeletal applications.
The transducer orientation marker should point to the right of the patient in transverse scanning and cranially/proximally in longitudinal axis scanning.
It is often helpful to have the patient pinpoint the area of concern or maximal tenderness to guide the exam.
Scan in a natural anatomic position for examining most musculoskeletal structures—awkward or uncomfortable positions can cause fatigue and decrease scanning quality.
Use contralateral, unaffected structures for comparison to the symptomatic side.
In challenging areas such as the wrist or joints, first identify an anatomical point of reference, such as the hyperechoic cortical lines of known bony structures, and then subsequently identify adjacent tendons, ligaments, and muscles.
To best view the shoulder joint, consider using a curvilinear transducer. Align the transducer parallel and just inferior to the scapular spine, and slide the transducer out laterally until you are centered on the humeral head and glenoid.
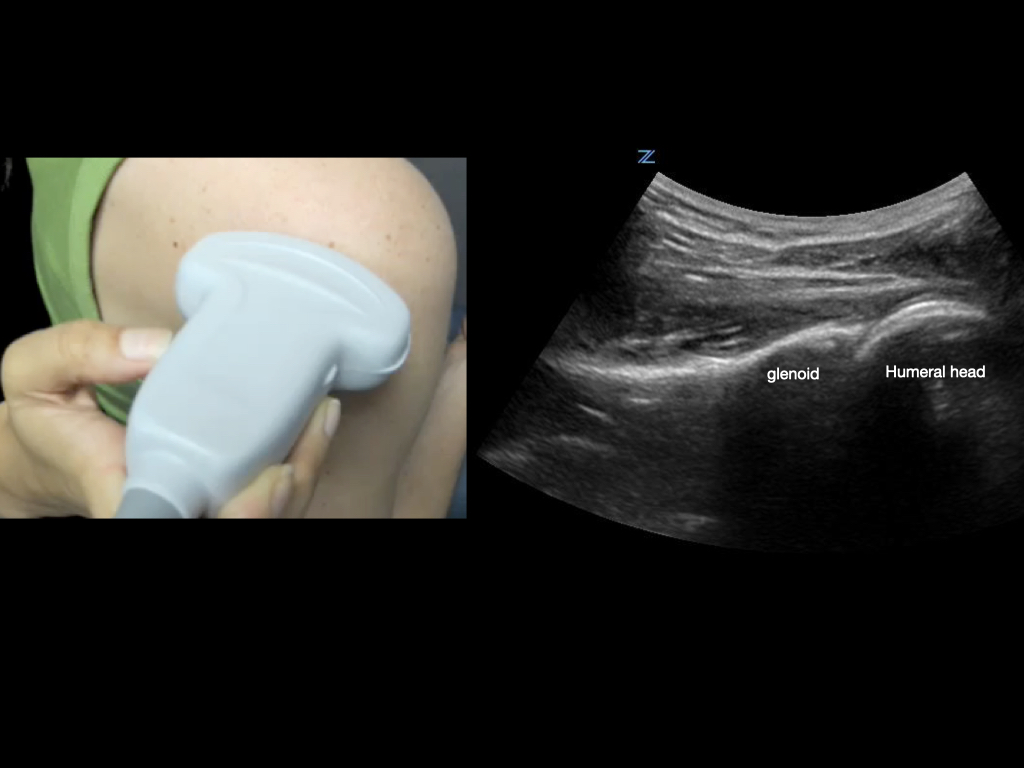
Figure 4.
Transducer orientation when scanning the glenohumeral joint.
For very superficial structures, consider using a standoff pad, copious amounts of gel, or a water bath. This can also help decrease pressure applied to painful areas. Water baths are especially useful for hands and feet, eg, looking for foreign bodies.
Video 3.
Demonstration of water bath technique: place the hand in a water bath and hover a high frequency linear transducer over the tendon in question – in this case, a flexor tendon of the hand; have the patient flex the digit or other attached structure while observing the ultrasound screen.
Video 4.
Short axis of finger moving distal to proximal using water bath technique.
Take advantage of dynamic exams. For example, observe tendons moving through their range of motion; have the shoulder internally and externally rotate to observe the humeral head in the glenoid when evaluating for dislocation, etc.
Video 5.
Tendon range of motion imaging: Observe the flexor tendon sliding along its path. Look for discontinuities such as complete tears with a severed end sliding into view, or partial tears as a dark or ragged section in a focal area of the tendon.
Video 6.
Posterior shoulder internal and external rotation. This view (corresponding to Figure 4) shows the posterior humeral head rotating in the glenoid, confirming shoulder reduction, and demonstrating the rotator cuff tendon in motion.
Keep the exam simple and limited – most pathology the emergency physician aims to find will be marked either by a visible disruption, abnormal fluid, or both.
Anisotrop
Anisotropic artifacts can significantly impact the accuracy of ultrasound imaging, particularly in musculoskeletal and nerve evaluations. The key to managing anisotropy is understanding its causes and actively compensating for it during scanning. When scanning tendons or nerves, the sonographer should employ a dynamic scanning technique, continually adjusting the angle of the transducer to maintain perpendicularity to the target structure. This approach helps maintain the echogenicity and clarity of the structure, reducing the risk of misinterpretation. Additionally, it is crucial to correlate sonographic findings with clinical presentation and, if necessary, compare images with contralateral structures to differentiate between true pathological changes and artifacts. Utilizing color Doppler can also aid in distinguishing between vascular and nonvascular structures, as true tendinopathy or nerve pathology may not demonstrate vascular flow, while anisotropic areas typically do not have blood flow. These strategies collectively enhance the diagnostic accuracy of ultrasound examinations, ensuring that anisotropy does not lead to misdiagnosis or inappropriate clinical decisions.
Video 7.
Anisotropy artifacts:
Demonstrating angling of the transducer over the median nerve of the forearm.
Video 7b.
Anisotropy artifacts:
The resultant artifact when viewed in the short axis
Video 7c.
Anisotropy artifacts:
Similar anisotropic effect seen on palmar tendons in the short axis. When the transducer is not perpendicular to the tendon or nerve, the structure darkens and loses the bright fibrillar/punctate pattern (honeycomb-like appearance for nerves) that makes them recognizable.
4. Pathology
Fractures
Appear as a sharp discontinuity in the bright line of the bony cortex on ultrasound.
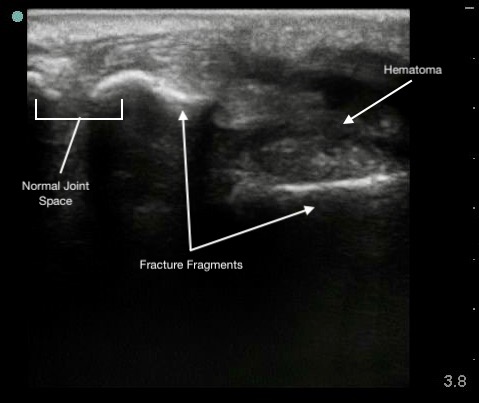
Figure 6.
Colles (distal radius) fracture.
Figure 7a.
its corresponding CT
(Note: I saw no image for this)
Figure 7b.
Comminuted sternal fracture A) on ultrasound
(Note: I saw no image for this)
Video 8.
Sternal fracture moving with respiration.
Hypoechoic hematoma or effusion may be visible in the surrounding soft tissue.
Ultrasound allows immediate assessment of the presence and extent of a fracture at the area of tenderness.
Capable of detecting displacement as small as 1 mm.
Less effective for evaluating fracture geometry or comminution.
Ultrasound guidance can enhance the effectiveness of hematoma blocks by ensuring accurate anesthetic delivery.
Advanced uses include:
- Detecting occult fractures.
- Identifying small avulsion fractures.
- Guiding fracture reductions.
Easier to identify fractures in long bones (eg, distal radius, femur, clavicle) than in smaller bones (eg, carpals).
Point-of-care ultrasound (POCUS) offers higher sensitivity for detecting rib and sternal fractures compared to plain radiographs.13-18
Figure 5.
Longitudinal view of a rib fracture.
(Note: I saw no image for this)
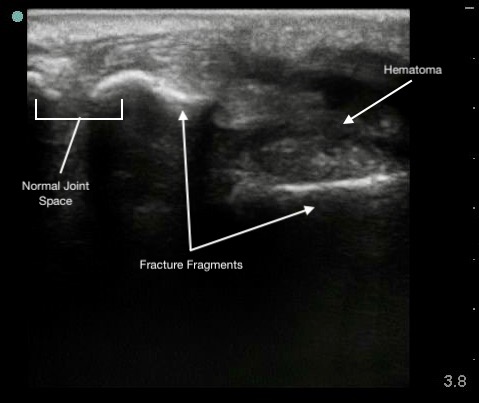
Figure 6.
Colles (distal radius) fracture.
Effusions
Appear as black (anechoic) areas within the joint space on ultrasound.

Figure 8.
A knee effusion seen with a linear transducer. Transducer positioning is the same as Figure 2C.
Presence of irregular internal echoes may indicate complex effusions due to:
- Hematoma.
- Pus.
- Fibrinous material.1
o POCUS is useful for guiding arthrocentesis, allowing precise aspiration of fluid from the joint space.3,5,9
Video 9.
Arthrocentesis of knee effusion
Shoulder Dislocation
Anterior Dislocation:
- The humeral head is displaced anterior to the glenoid.
- Appears at the bottom of the screen as the transducer is placed on the posterior shoulder.
- Movement is away from the transducer since the orientation is posterior-to-anterior.
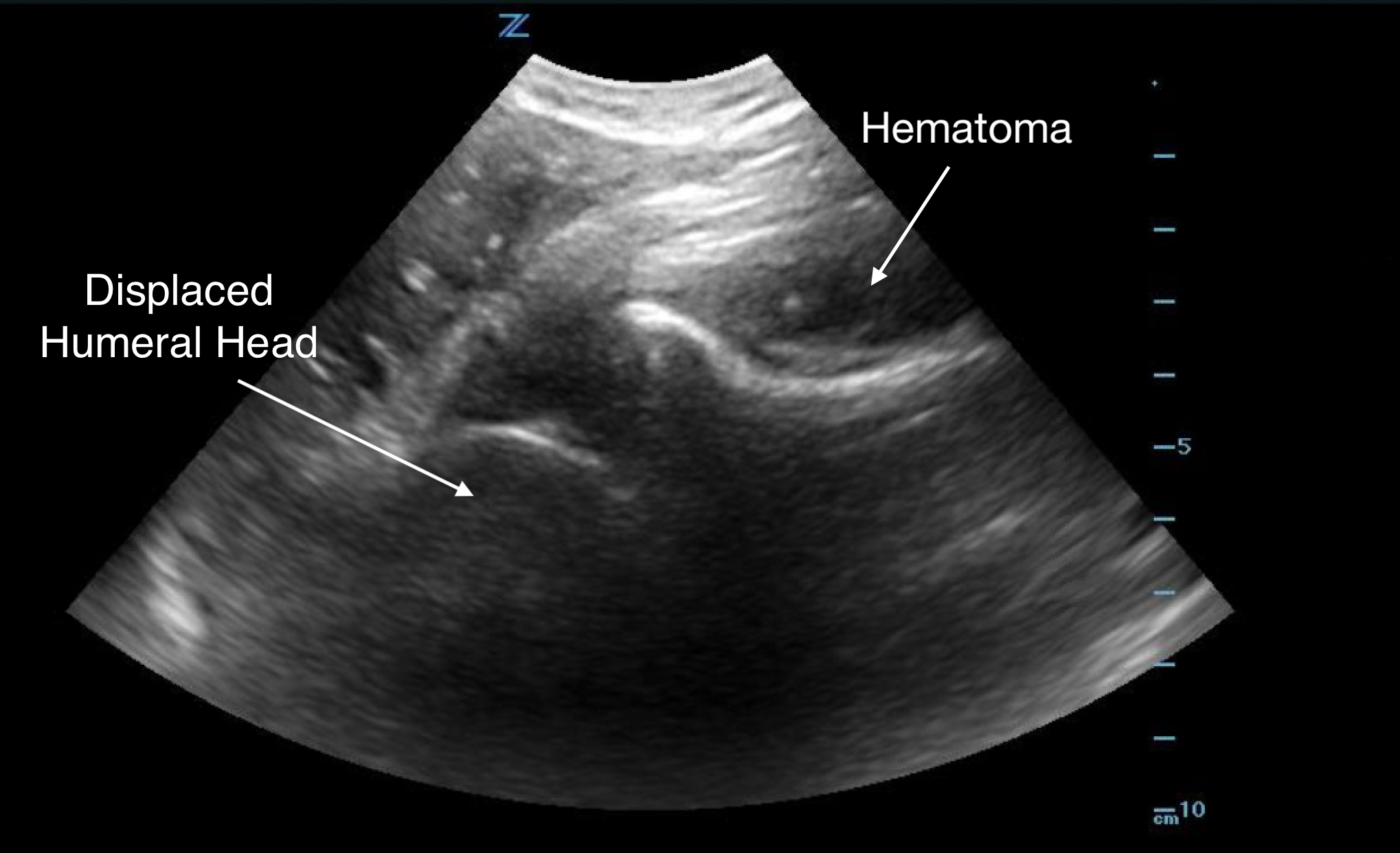
Figure 9.
Anterior shoulder dislocation with overlying hematoma
Posterior Dislocation:
- The humeral head moves towards the transducer.
- Ultrasound is particularly helpful in diagnosing posterior dislocations, which can be difficult to identify on radiographs.
- If unclear, compare with the unaffected shoulder for clarity.
- Ultrasound is effective in confirming a successful reduction of the dislocation.
Note: Ultrasound should not replace radiographs; it is essential to determine the presence of underlying fractures both before and after reduction. Each imaging modality has its best applications, and they complement each other in patient evaluation and management.
Soft Tissue
Abscesses and hematomas are readily identifiable on ultrasound as abnormal fluid collections in areas of tenderness or swelling. The appearance of the fluid varies depending on its contents, the presence of gas, and the clotting state of the hematoma. Fluid may appear anechoic (most common), heterogeneous, or even isoechoic. A key indicator in uncertain cases is the posterior acoustic enhancement generated by the fluid contents.

Figure 10.
Superficial abscess with posterior acoustic enhancement and surrounding cobblestoning (from cellulitis) deep to the abscess.
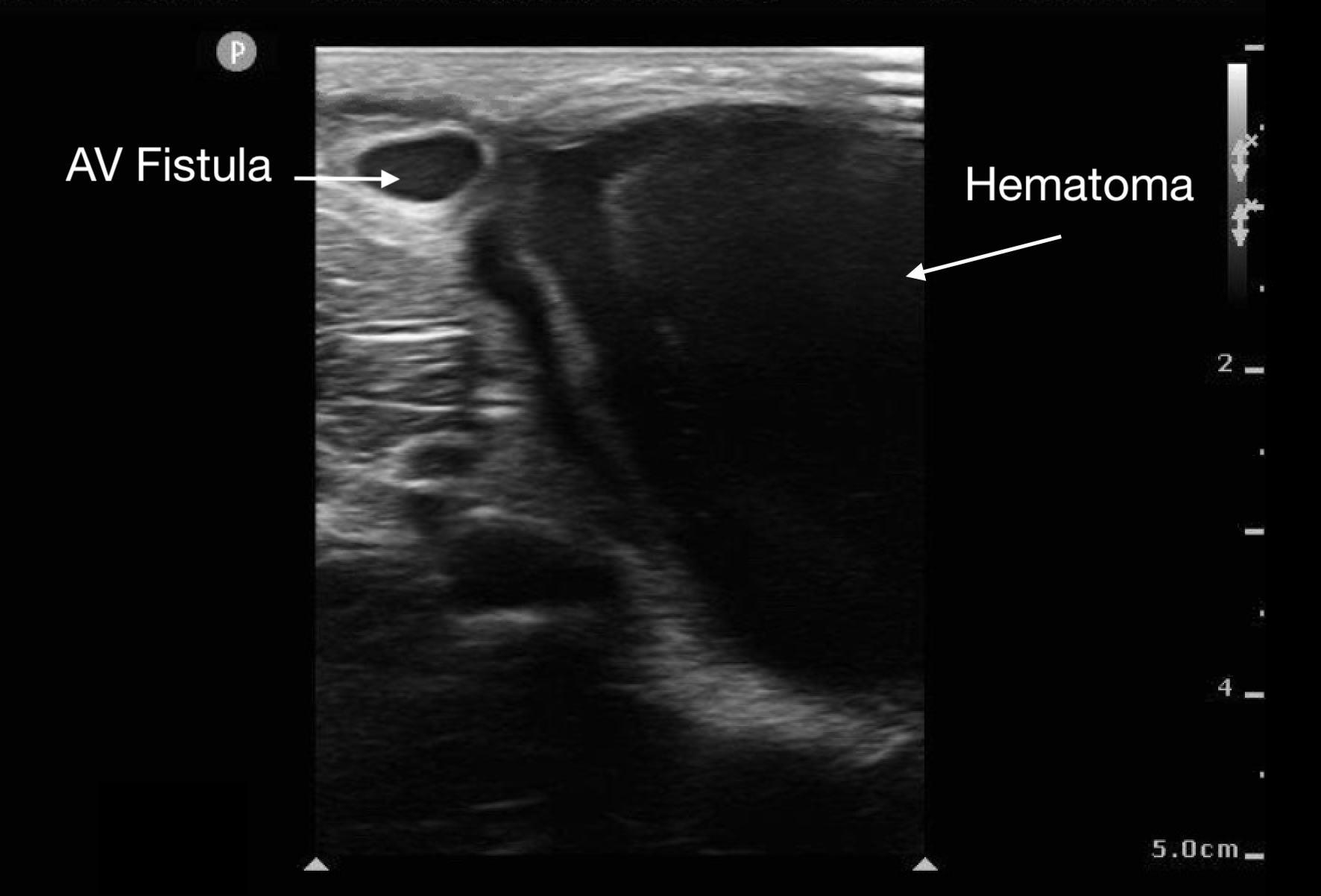
Figure 11.
Large hematoma from ruptured AV fistula seen in upper left corner of image.
Before draining an abscess, it is crucial to use color Doppler to rule out a pseudoaneurysm or nearby large vessels. This step helps prevent inadvertent incision into a vascular soft tissue structure, such as a lymph node, which may appear similar to an abscess.
Muscle, Tendon and Ligament Injuries
Muscle tears in biceps femoris, rectus femoris, and gastrocnemius will show a discontinuity in the muscle belly and adjacent hematoma. The associated “clapper in bell” sign is the retracted upper portion of torn muscle fibers (clapper) surrounded by hematoma (bell).19
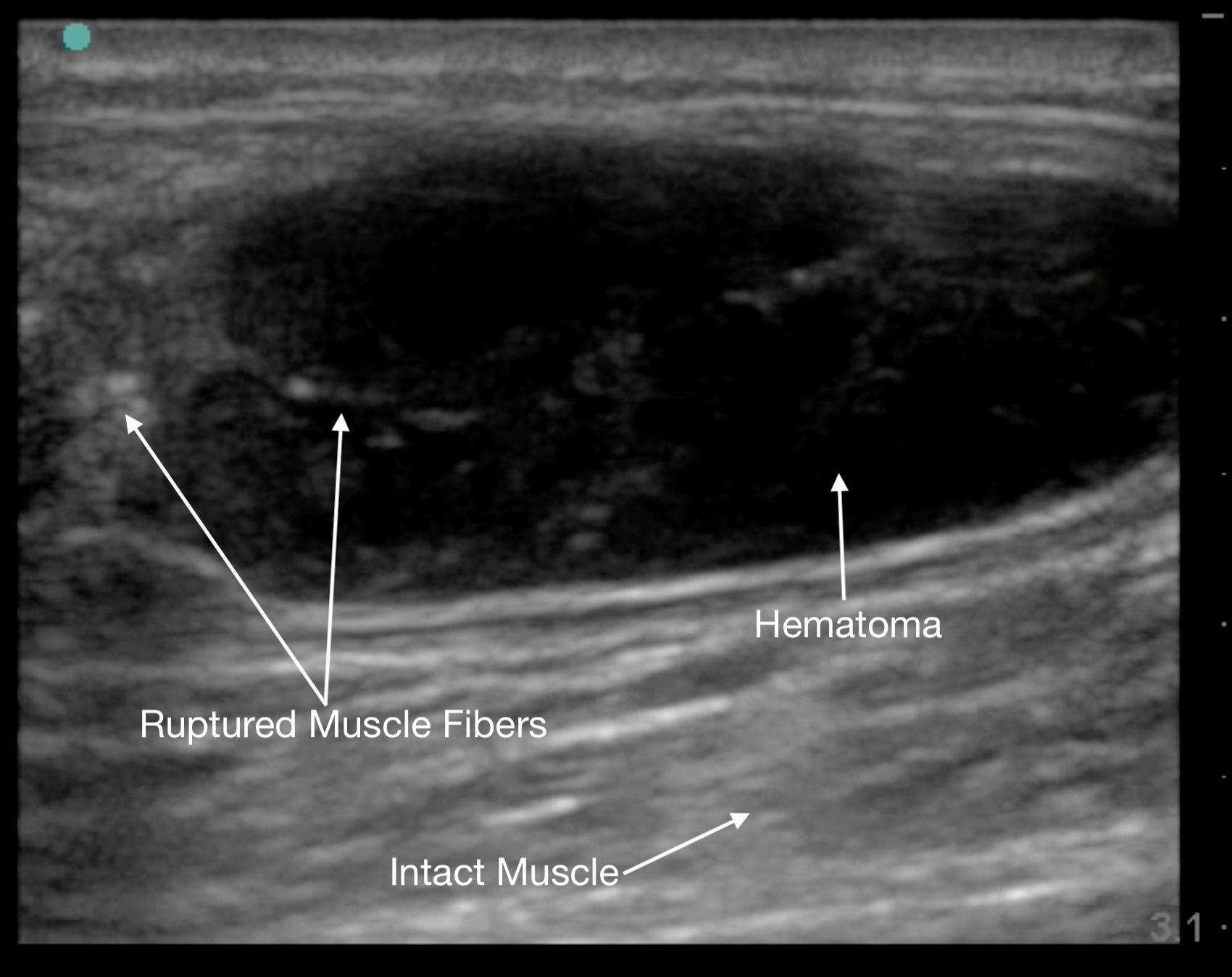
Figure 12.
Gastrocnemius muscle tear in short axis at its proximal end.
Tendon ruptures appear as areas of hypoechogenicity from edema/hematoma, and adjacent bunched up, retracted tendon fibers. For complete tears, the portion of the tendon near the injury will lose its rigid, straight appearance and instead appear irregular and have a large gap between the torn end and its insertion point. Partial tears are more subtle and will sometimes only have a small, cone-shaped hypoechoic focus. The key with tendon exams is to view them dynamically, having the patient flex and extend the injured joint (if possible).
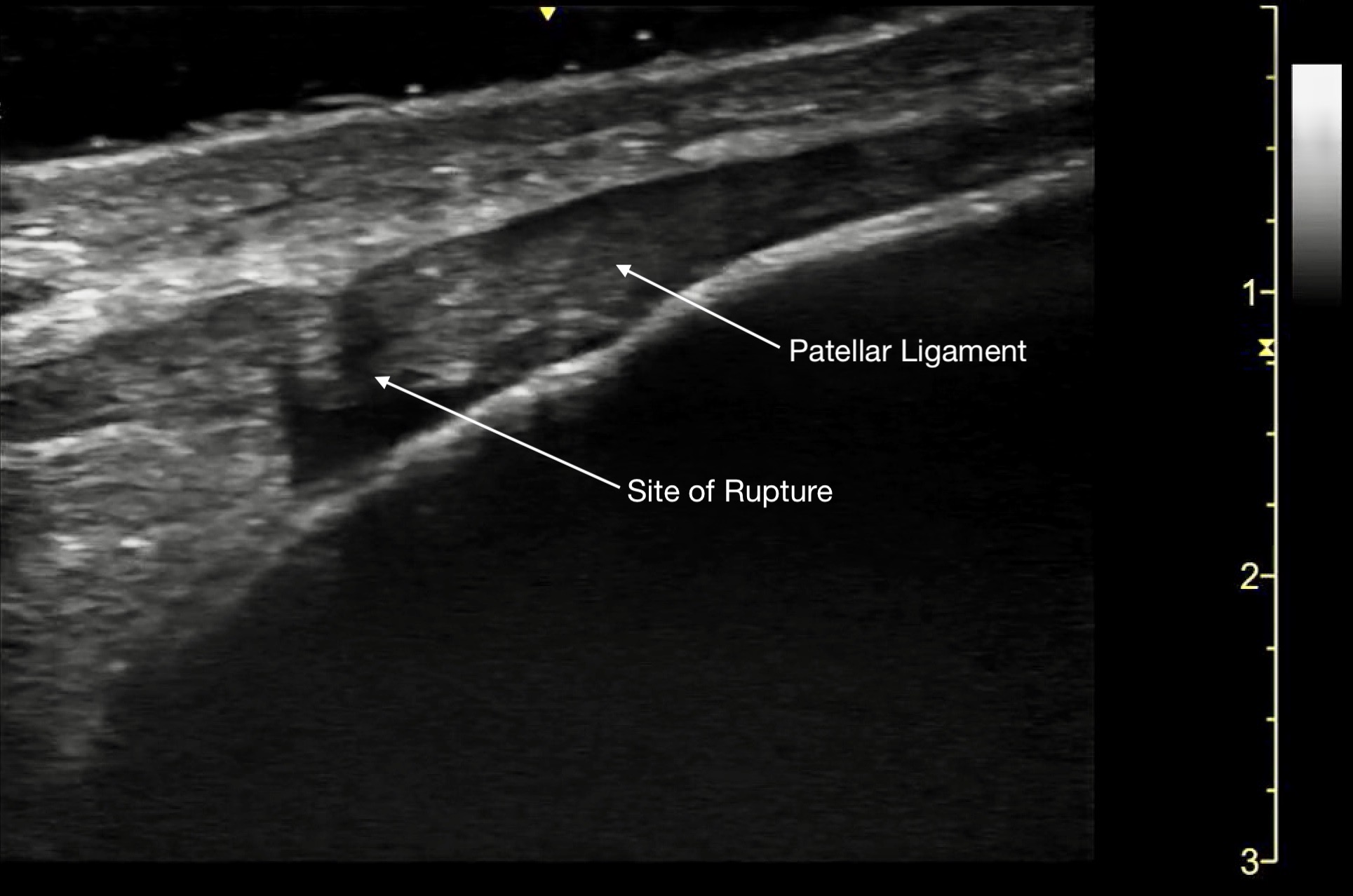
Figure 13a.
A) Partial rupture of the patellar ligament at the distal insertion
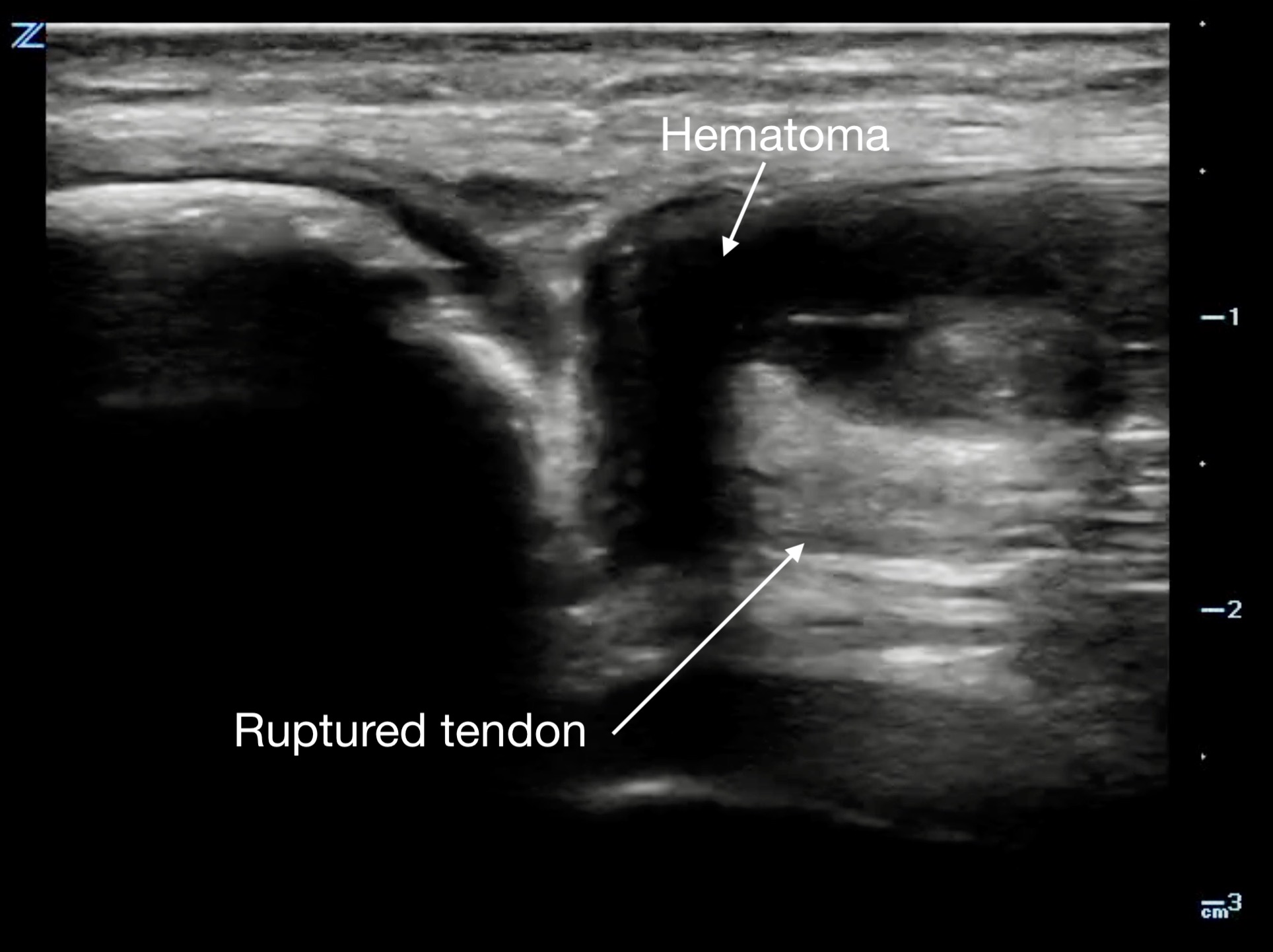
Figure 13b.
a different patient with a complete rupture at the proximal insertion of the patellar tendon. The patella is on the left side of the image, and note the hematoma that wraps around the ruptured end of the tendo
Video 10.
Partial rupture of the patellar ligament at the distal insertion, demonstrating the remaining intact portion when fanning across the ligament.
Tenosynovitis will appear as a thickened tendon and on short axis will have a halo of anechoic fluid surrounding it in the tendon sheath.
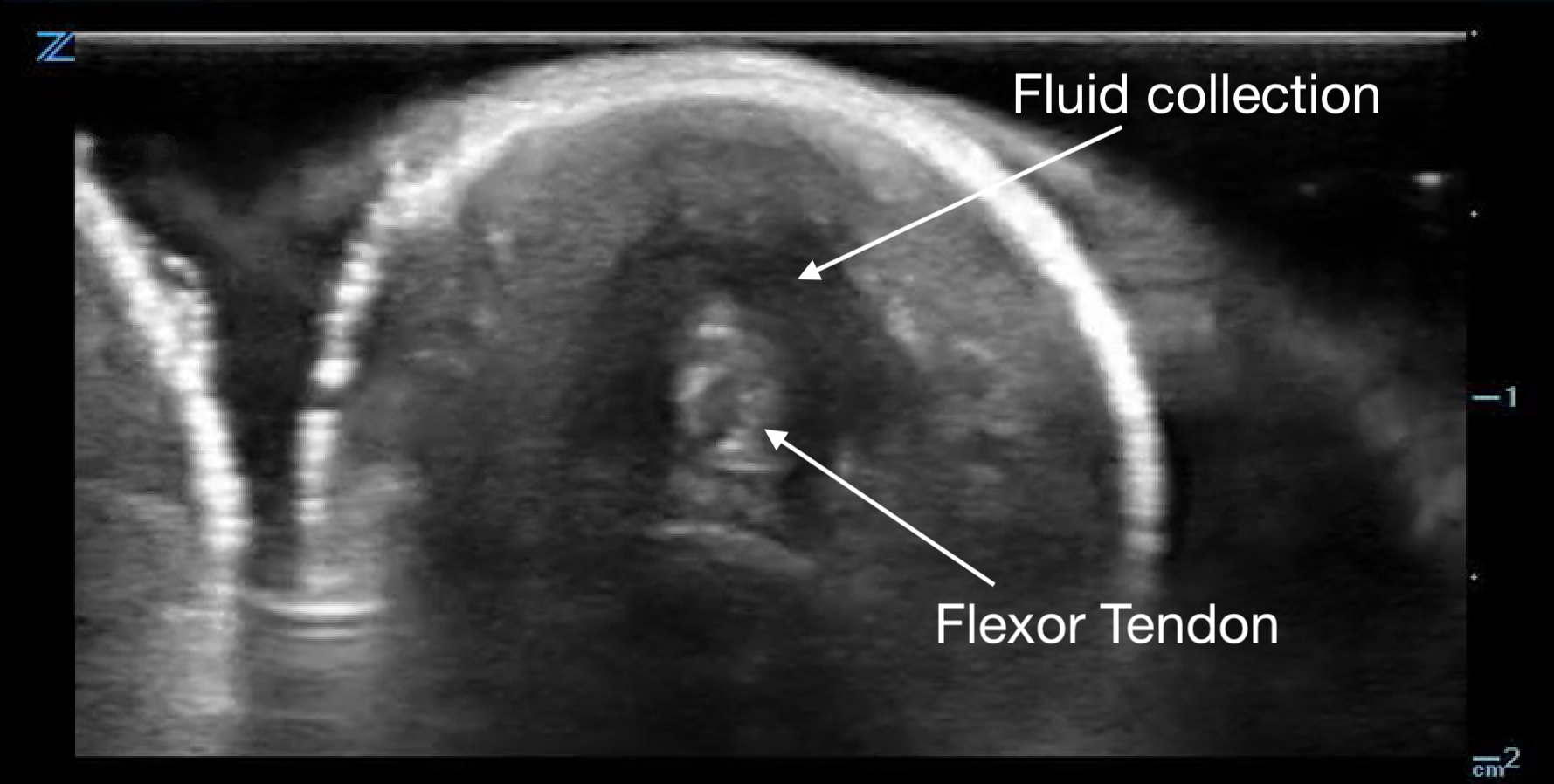
Figure 14a.
Flexor tenosynovitis demonstrated by the halo of fluid in the sheath surrounding the tendon
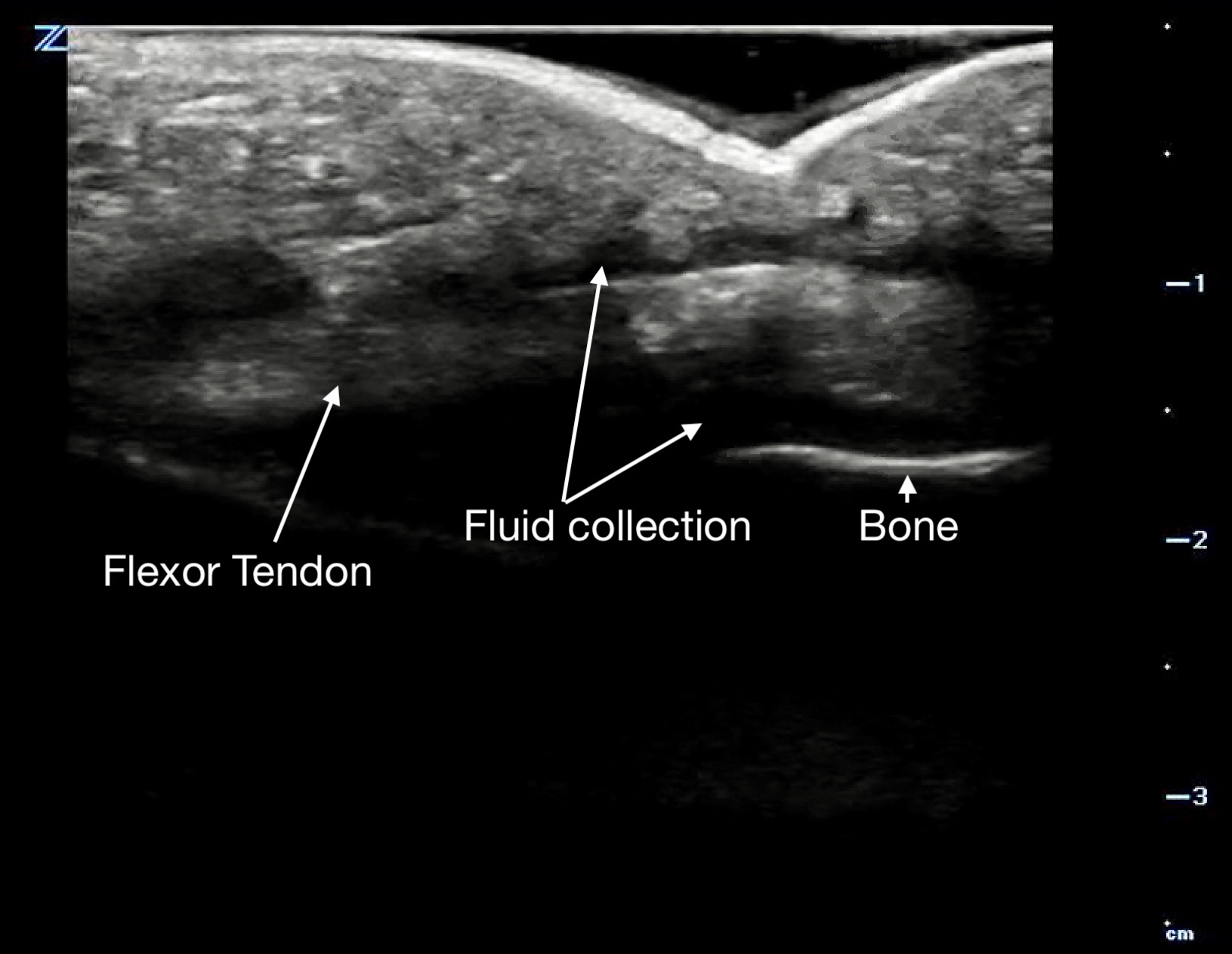
Figure 14b.
a long axis view with fluid above and below the flexor tendon.
5 Pearls and Pitfalls
- Failure to compare to normal contralateral anatomy
- Failure to observe structures throughout their dynamic range when possible
- Failure to set up the exam beforehand so as to be comfortable for both patient and sonographer.
- Failure to account for anisotropy in the study of tendons and nerves
- Use copious gel or stand-off pad over superficial, painful, or topographically convoluted surfaces
- Scan all structures in two planes - longitudinal and transverse
- Failure to know one’s limits and that of the tools you use
6. References
- Valley VT, Stahmer SA. Targeted musculoarticular sonography in the detection of joint effusions. Acad Emerg Med. 2001;8:361-367.
- Tayal VS, Antoniazzi J, Pariyadath M, Norton HJ. Prospective use of ultrasound imaging to detect bony hand injuries in adults. J Ultrasound Med. 2007;26(9):1143‐1148.
- Freeman K, Dewitz A, Baker W. Ultrasound guided hip arthrocentesis in the ED. Am J Emerg Med. 2007;25:80-86.
- LaRocco BG, Zlupko G, Sierzenski P. Ultrasound diagnosis of quadriceps tendon rupture. J Emerg Med. 2008;35:293-295.
- Roy S, Dewitz A, Paul I. Ultrasound-assisted ankle arthrocentesis. Am J Emerg Med. 1999;17:300-301.
- Canagasabey MD, Callaghan MJ, Carley S. The Sonographic Ottawa Foot and Ankle Rules Study (the SOFAR Study). Emerg Med J. 2011;28(10):838-40.
- Adhikari S, Blaivas M, Lander L. Comparison of bedside ultrasound and panorex radiography in the diagnosis of a dental abscess in the ED. Am J Emerg Med. 2011;29(7):790-5.
- laton A, Poletti PA, Van Aaken J, Fusetti C, Della Santa D, Beaulieu JY, Becker CD. Occult fractures of the scaphoid: the role of ultrasonography in the emergency department. Skeletal Radiol. 2011 Jan 1.
- Wiler JL, Costantino TG, Filippone L, Satz W. Comparison of ultrasound-guided and standard landmark techniques for knee arthrocentesis. J Emerg Med. 2010;39(1):76-82.
- 1Costantino TG, Roemer B, Leber EH. Septic arthritis and bursitis: emergency ultrasound can facilitate diagnosis. J Emerg Med. 2007;32(3):295-7.
- Bücklein W. [Emergency ultrasound diagnosis of the musculoskeletal system]. Rontgenpraxis. 1999;52(3-4):103-9. Review. German.
- American College of Emergency Physicans. Ultrasound Guidelines: Emergency, Point-of-Care, and Clinical Ultrasound Guidelines in Medicine [policy statement]. Approved by the ACEP Board, April 2023. Accessed September 2025.
- Pourmand A, Shokoohi H, Maracheril R. Diagnostic accuracy of point-of-care ultrasound in detecting upper and lower extremity fractures: An evidence-based approach. Am J Emerg Med. 2018;36(1):134-6.
- Griffith JF, Rainer TH, Ching AS, Law KL, Cocks RA, Metreweli C. Sonography compared with radiography in revealing acute rib fracture. AJR Am J Roentgenol. 1999;173:1603-9.
- Jin W, Yang DM, Kim HC, Ryu KN. Diagnostic values of sonography for assessment of sternal fractures compared with conventional radiography and bone scans. J Ultrasound Med. 2006;25(10):1263-8.
- You JS, Chung YE, Kim D, Park S, Chung SP. Role of sonography in the emergency room to diagnose sternal fractures. J Clin Ultrasound. 2010;38(3):135-7.
- 17. McNeil CR, McManus J, Mehta S. The accuracy of portable ultrasonography to diagnose fractures in an austere environment. Prehosp Emerg Care. 2009;13(1):50-2.
- Marshburn TH, Legome E, Sargsyan A, Li SM, Noble VA, Dulchavsky SA, Sims C, Robinson D. Goal-directed ultrasound in the detection of long-bone fractures. J Trauma. 2004;57(2):329-32.
- Jacobson, Jon A. Fundamentals of Musculoskeletal Ultrasound. Philadelphia, PA: Saunders/Elsevier, 2007. Print.
- Dewitz A. Chapter 18. Musculoskeletal, Soft Tissue, and Miscellaneous Applications. In: Ma O, Mateer JR, Reardon RF, Joing SA. eds. Ma and Mateer's Emergency Ultrasound, 3e New York, NY: McGraw-Hill.
- Boswell B, Farrow R, Rosselli M, Farcy DA, Santana L, Santos CD, Cubeddu LX. Emergency Medicine Resident-Driven Point of Care Ultrasound for Suspected Shoulder Dislocation. South Med J. 2019;112(12):605-9.
- Abrams M, Magee MA, Risler Z, Lewiss RE, Au AK. Unorthodox Use of Point-of-care Ultrasound to Evaluate Seizures. Cureus. 2019;11(1):e3960.
- Gottlieb M, Holladay D, Peksa GD. Point-of-care ultrasound for the diagnosis of shoulder dislocation: A systematic review and meta-analysis. Am J Emerg Med. 2019;37(4):757-61.[JR1]