Supraclavicular Brachial Plexus Block
Leonard V. Bunting, MD, FACEP
I. Introduction and Indications
- The supraclavicular block is a powerful technique that is well tolerated by patients in the ED.1,2
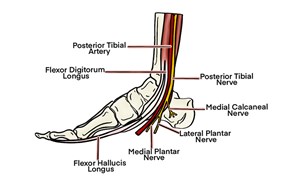
- Covers common areas of injury. (Illustration 1)
- Superficial placement and clear landmarks make for easier needle placement.
- Lower risk of phrenic nerve involvement than the interscalene block
Indications
- Management of painful conditions of the arm below the shoulder (burns, fractures, dislocations, infections).
- Procedural anesthesia for reduction of the elbow or wrist and manipulation of fractures of the humerus, elbow, forearm or wrist.
Contraindications
- General block contraindications
- Lung disease or debility (may cause ipsilateral diaphragm paralysis)
- Injuries involving the shoulder
- Injuries isolated to the hand
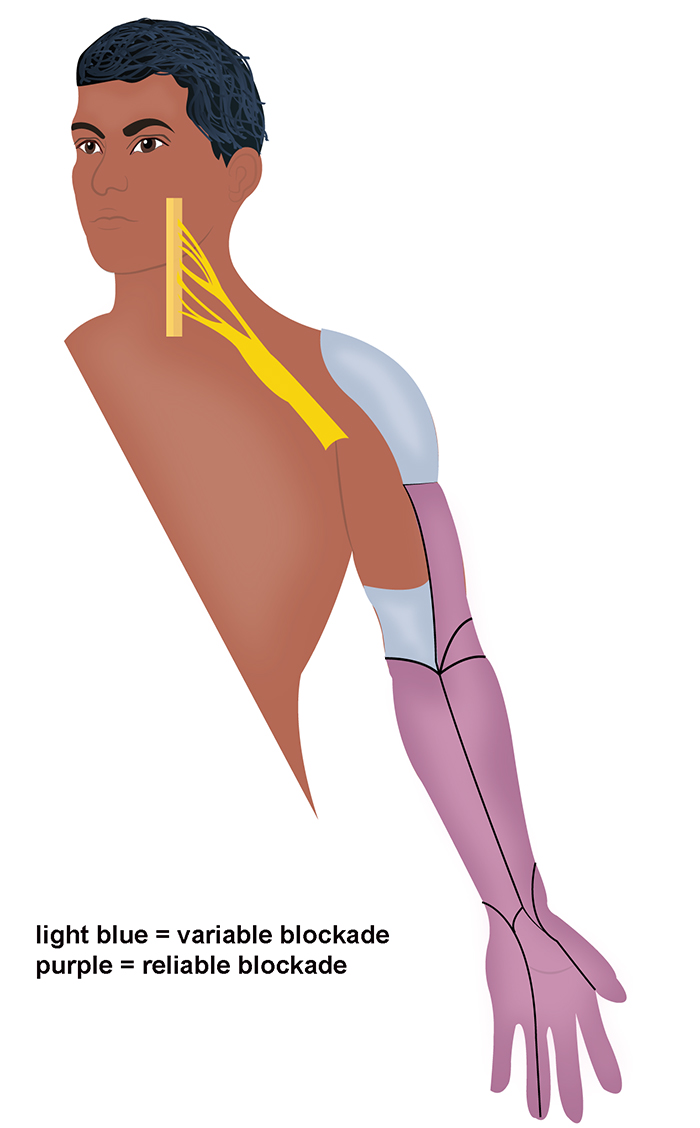
Illustration 1. Anterior and posterior distribution of anesthesia
II. Equipment
- Skin prep and sterile probe cover
- 8-12 MHz linear array probe
- 27-gauge needle and syringe of 3-5 cc of 1% lidocaine with epi for skin anesthesia
- 3.5-inch, 22-gauge spinal needle
- 30cc syringe with local anesthetic of choice
III. Setup and Patient Positioning
- General procedure setup
- Ultrasound machine is usually placed on the opposite side of the bed from the block site.
- Patient is positioned supine or semi-recumbent with their head rotated 45 degrees to the contralateral side.
- If the stretcher prevents free movement of the block needle, place a pillow or large towel roll behind the ipsilateral shoulder or shift the patient closer to the ipsilateral side of the mattress to create free space behind the block site.
- If the needle and syringe are too large to comfortably manipulate, consider extension tubing between the syringe and needle to decrease space needed at the block site.
IV. Pre-scan and Sonographic Anatomy
- Anatomy
- The supraclavicular fossa is a depression superior to the clavicle.
- Underneath this fossa is an anatomic space called the supraclavicular space, which contains the subclavian artery, brachial plexus, first rib and dome of the lung.
- The brachial plexus enters the supraclavicular fossa from the interscalene space and lies superior & posterior to the subclavian artery.
- Inferior to the subclavian artery, the first rib and dome of the lung form the floor of the supraclavicular space.
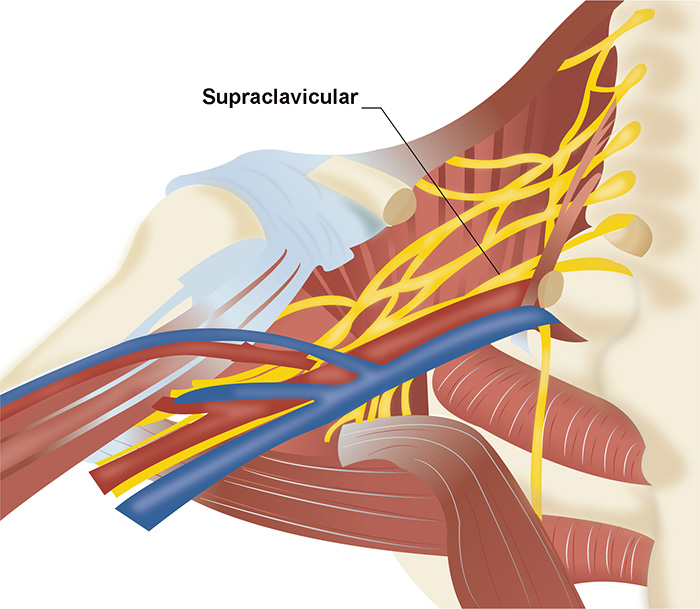
Illustration 2. Anatomy of the supraclavicular fossa
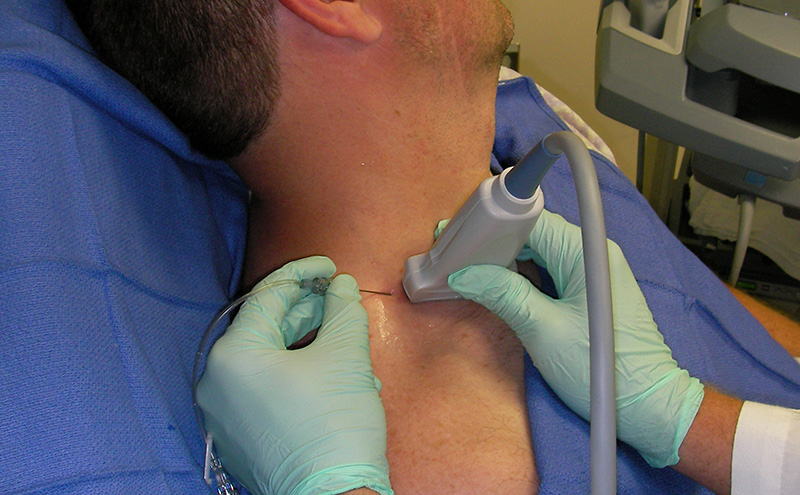
- Place a high-frequency linear array probe in the supraclavicular fossa perpendicular to the mid-clavicle. (Figure 1)
- Orient probe indicator to the operator’s left.
- Set depth to 4-6 cm depending on patient’s body habitus
- Obtain a cross-section view of the subclavian artery, identified by its thick wall and brisk pulsations. Color-flow is rarely needed but may be used.
- Identify the brachial plexus abutting the superior-posterior wall of the subclavian artery and is seen as a grouping of small hyperechoic circles with hypoechoic centers, similar to a bunch of grapes.
- Deep to the artery note the dome of the lung (identified by its characteristic movement and scatter) and the first rib (identified by its hyperechoic surface with dense posterior shadowing).
Video 1. Pre-scan for the supraclavicular block
V. Technique
- In-plane approach from the osterior side of the probe is performed
- Probe indicator oriented to operator’s left
- Center the brachial plexus on the image
- Anesthetize the block site with a skin wheal
- Insert the block needle 1 cm at ~45 degrees to the skin surface
- Visualize the needle and ensure it is always in view
- Slowly advance the needle towards the deep, proximal border of the plexus where it meets the subclavian artery
- Once movement of the needle causes movement on the plexus, injection may begin
- Follow injection precautions.
- Initially inject 0.5 cc.
- Appropriate needle placement is confirmed by anesthetic flowing around the entire plexus and dissecting the plexus from the artery.
- Typical block volumes are 30-45 ml.3
- Readjustment of the needle position may be necessary to achieve adequate distribution of anesthesia.
- Always perform aspiration and incremental injection to avoid systemic distribution of the anesthetic.
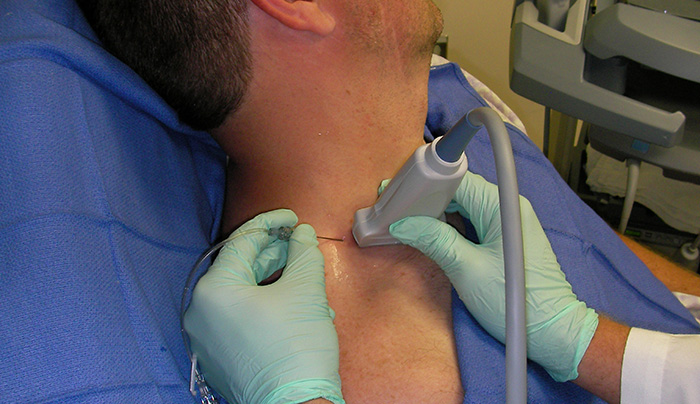
Figure 1. In-plane needle placement
Video 2. Supraclavicular nerve block
VI. Pearls and Pitfalls
- The brachial plexus in the supraclavicular fossa does not travel parallel to the skin surface. Therefore, due to anisotropy, it may be necessary to alter the probe's angle to the skin to optimally visualize the plexus.
- Corner Pocket Approach - A popular initial target for injection is the area inferior to the plexus, posterior to the subclavian artery and superior to the first rib, commonly referred to as the corner pocket. Although an easy initial target, one study found an unacceptably high rate of ulnar sparing using this approach.3 Therefore, regardless of the initial needle placement, it is recommended that the needle be redirected as needed to ensure the entire plexus is surrounded by local anesthetic.
- To help find the brachial plexus and the optimal site for injection, rapidly slide the probe on the lateral aspect of the neck.
Video 3. Interscalene to supraclavicular plexus transition
This approach has three additional complications that should be noted:
- Although the phrenic nerve is much further from the block site than in the interscalene approach, ipsilateral diaphragm paralysis still occurs in 50% of cases.4 In one case series, this was rarely symptomatic.5 Minimizing the amount of LA used may decrease the likelihood of this complication.6
- The proximity of the lung makes a pneumothorax possible. In large case series, no symptomatic pneumothoraces occurred,7 but individual cases have been reported.8
- A temporary Horner’s syndrome may result from proximal LA spread and blockage of sympathetic afferents.7 This is self-limited and will resolve as the block resolves.
VII. References
- Stone MB, Wang R, Price DD. Ultrasound-guided supraclavicular brachial plexus nerve block vs procedural sedation for the treatment of upper extremity emergencies. Am J Emerg Med. 2008;26:706-10.
- Stone MB, Price DD, Wang R. Ultrasound-guided supraclavicular block for the treatment of upper extremity fractures, dislocations, and abscesses in the ED. Am J Emerg Med. 2006;25:472-5.
- Fredrickson MJ, Patel A, Young S, Chinchanwala S. Speed of onset of 'corner pocket supraclavicular' and infraclavicular ultrasound guided brachial plexus block: a randomised observer-blinded comparison. Anaesthesia. 2009;64(7):738-44.
- Franco C: Supraclavicular Brachial Plexus Block. In Hadzic A (ed): Textbook of Regional Anesthesia. McGraw-Hill, 2007, p 424.
- Perles A, Lobo G, Lo N, Brull R, Chan VWS, Karkhanis R. Ultrasound-guided supraclavicular block: outcome of 510 consecutive cases. Reg Anesth Pain Med. 2009;34(2):171-6.